¿Cuándo empezaré a ver el crecimiento del colágeno? después de la microaguja?
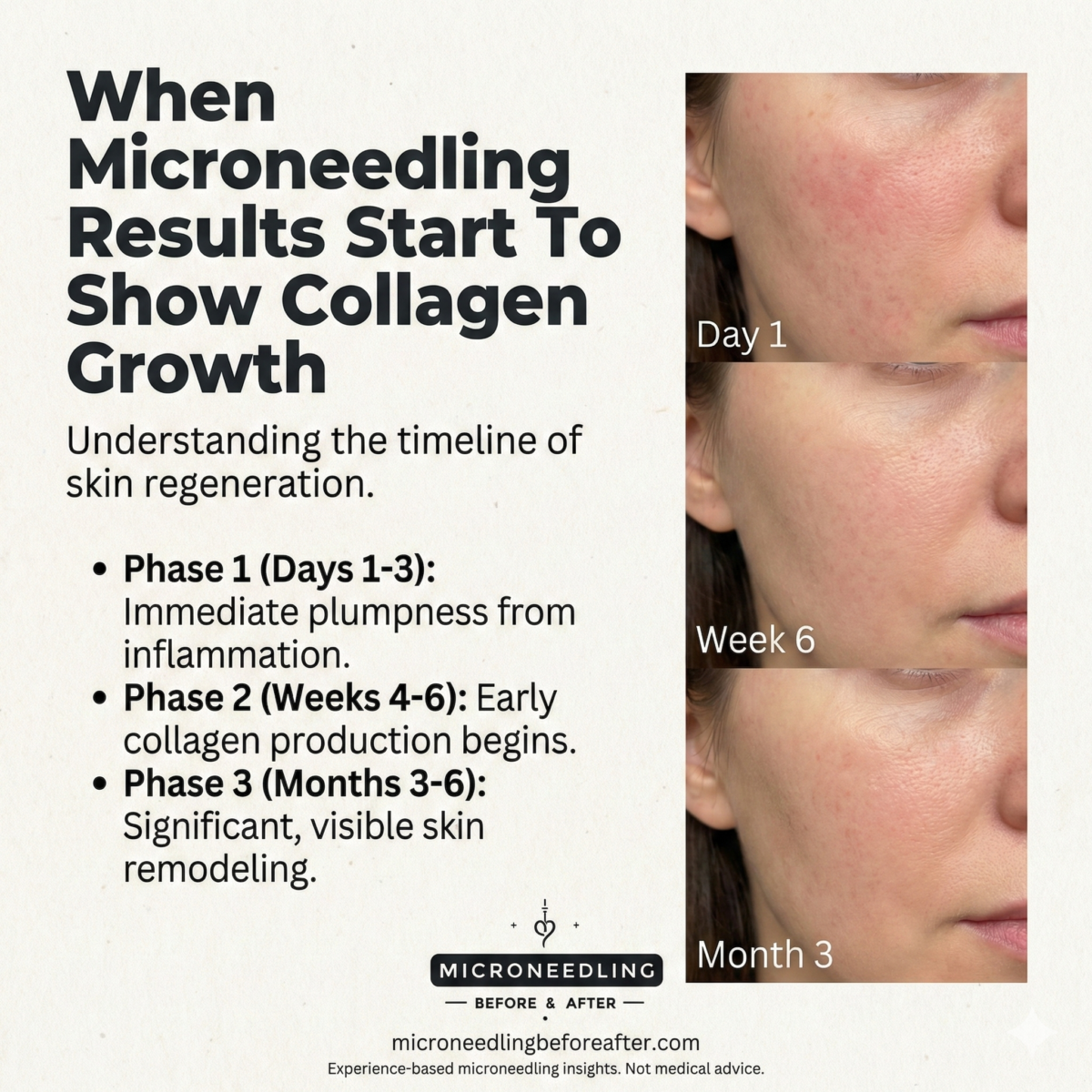
Cuando los resultados de la microaguja comienzan a mostrar crecimiento de colágeno
Escribí este artículo para aclarar la cronología y los mecanismos mediante los cuales la microaguja desencadena la producción de colágeno. Explicaré qué esperar, por qué varían los resultados y cómo supervisar y apoyar el proceso para obtener el mejor resultado clínico.
Qué cubre este artículo
Describiré la respuesta biológica a la microaguja, proporcionaré un cronograma basado en la evidencia para la síntesis de colágeno y los resultados visibles, e identificaré las variables que alteran significativamente los resultados. También describiré las técnicas de monitorización, los cuidados posteriores adecuados y recomendaciones prácticas para optimizar la producción de colágeno de forma segura.
Cómo la microaguja estimula la producción de colágeno
Considero la microaguja como una lesión dérmica controlada que activa intencionalmente las vías de cicatrización. Al crear múltiples microcanales en la piel, el procedimiento inicia una cascada inflamatoria y la liberación de factores de crecimiento que, en última instancia, estimulan a los fibroblastos a sintetizar nuevo colágeno y matriz extracelular.
Las tres fases de la cicatrización de heridas relevantes para la microaguja
El proceso de cicatrización de heridas se produce en fases superpuestas: inflamación, proliferación y remodelación. Resumiré cada fase y su función en la síntesis de colágeno para que comprendas por qué los cambios visibles tardan semanas o meses.
- Inflamación: Inmediatamente después del tratamiento, las plaquetas liberan factores de crecimiento y las células inmunitarias eliminan los residuos. Cabe destacar que esta fase prepara el terreno para la activación de los fibroblastos, pero no produce una cantidad significativa de colágeno visible.
- Proliferación: Los fibroblastos proliferan y comienzan a depositar colágeno tipo III y glicosaminoglicanos. Observo que esta fase suele durar días o semanas y es cuando se producen los primeros cambios en la matriz extracelular.
- Remodelación: El colágeno tipo III se reemplaza gradualmente por colágeno tipo I, más fuerte, y las fibras de colágeno se reorganizan. Cabe destacar que la remodelación puede continuar durante meses, por lo que los pacientes suelen notar una mejoría progresiva con el tiempo.
Respuesta cutánea inmediata y qué significa
Inmediatamente después de la microaguja, preveo eritema, inflamación leve y sangrado localizado en algunos casos. Estos signos indican activación vascular e inflamatoria, pero no son evidencia directa de la formación de nuevo colágeno en ese momento.
La importancia del eritema y las microlesiones
El eritema refleja un aumento del flujo sanguíneo y la liberación de mediadores inflamatorios, necesarios para la cicatrización. Cabe destacar que esta respuesta aguda es un prerrequisito para la síntesis de colágeno, pero es independiente de los cambios estructurales del colágeno que ocurren posteriormente.
Cómo las señales bioquímicas tempranas predicen la formación posterior de colágeno
Factores de crecimiento como el TGF-β, el PDGF y el VEGF se regulan positivamente en cuestión de horas o días tras la lesión. Describo que estas moléculas de señalización reclutan y activan fibroblastos, proporcionando el entorno bioquímico para la deposición de colágeno durante las semanas siguientes.
Cronograma típico para el crecimiento del colágeno después de la microaguja.
Presentaré una cronología práctica que médicos y pacientes pueden usar para establecer expectativas. Esta cronología combina la biología celular con observaciones clínicas de ensayos clínicos y la práctica clínica.
Semana 0-1: Reacción inmediata y señalización temprana
Durante la primera semana, se espera una inflamación aguda y reepitelización de la epidermis. Aclaro que, si bien los factores de crecimiento aumentan durante este intervalo, aún no se ha producido una deposición apreciable de colágeno en cantidades clínicamente visibles.
Semanas 1 a 4: Actividad temprana de fibroblastos y deposición inicial de matriz
Entre una y cuatro semanas, los fibroblastos comienzan a sintetizar colágeno, principalmente colágeno tipo III, y aparecen nuevos componentes de la matriz extracelular. Observo que se están produciendo cambios microscópicos, y algunos pacientes pueden notar mejoras sutiles en la textura de la piel o una reducción de las líneas de expresión en esta etapa.
Semanas 4 a 8: Aumento de la síntesis de colágeno y remodelación temprana.
Al cabo de uno o dos meses, preveo que la deposición de colágeno aumentará y comenzará la remodelación inicial de las fibras de colágeno. Explico que la mejoría clínica se hace más notoria en muchos pacientes durante este periodo.
Semanas 8 a 12: remodelación continua y ganancias estéticas visibles
Entre los dos y tres meses, suelo observar mejoras apreciables en la firmeza, las líneas de expresión y la uniformidad del tono de la piel. Cabe destacar que el colágeno tipo III está en transición hacia el colágeno tipo I, más fuerte, y la arquitectura de la matriz dérmica se vuelve más organizada.
3 a 6 meses y más: remodelación a largo plazo y resultados máximos
Les digo a mis pacientes que las mejoras más duraderas suelen aparecer entre tres y seis meses y pueden continuar hasta un año después del tratamiento. Recalco que la remodelación final del colágeno y el fortalecimiento de la estructura dérmica pueden tardar varios meses, por lo que es necesario tener paciencia.
Tabla de cronología: actividad esperada del colágeno y signos clínicos
Incluyo una tabla concisa para resumir la línea de tiempo para que los lectores puedan consultar rápidamente los eventos celulares esperados y las observaciones clínicas.
| Periodo de tiempo | Eventos celulares | Signos clínicos que podría observar |
|---|---|---|
| Inmediato (0–7 días) | Hemostasia, activación plaquetaria, liberación de factores de crecimiento. | Eritema, hinchazón, formación de costras, colágeno mínimo visible. |
| Temprano (1–4 semanas) | Reclutamiento de fibroblastos, comienza la deposición de colágeno tipo III | Mejora sutil de la textura, disminución de la rugosidad superficial. |
| Intermedio (4–8 semanas) | Aumento de la producción de colágeno, remodelación temprana. | Mejora notable en las líneas finas y comienza la firmeza de la piel. |
| Tardía (8 a 12 semanas) | Transición del colágeno tipo III al tipo I, reorganización de las fibras | Tensado continuo, elasticidad y tono mejorados. |
| A largo plazo (3 a 12 meses) | Remodelación y maduración continua del colágeno. | Beneficio clínico máximo, cambio estructural sostenido |
Factores que afectan la rapidez con la que crece el colágeno
Reconozco que el cronograma varía significativamente entre pacientes debido a factores intrínsecos y extrínsecos. Enumeraré y explicaré las variables más influyentes para que pueda evaluar expectativas realistas.
Edad del paciente y capacidad regenerativa intrínseca
La piel más joven generalmente se regenera más rápido y produce colágeno con mayor eficiencia. Explico que el envejecimiento reduce la actividad de los fibroblastos y la capacidad de respuesta de las células madre, lo que a menudo prolonga el tiempo hasta que se observan mejoras visibles relacionadas con el colágeno.
Tipo de piel, etnia y fotodaño basal
Los diferentes fototipos de piel y grados de fotoenvejecimiento influyen en la cicatrización y la respuesta del colágeno. Observo que la piel muy fotoenvejecida puede requerir más tratamientos y un período de remodelación más prolongado para lograr resultados similares a los de la piel menos dañada.
Profundidad del tratamiento y longitud de la aguja
La profundidad de la aguja juega un papel clave en el grado de lesión dérmica y el estímulo de colágeno resultante. Proporciono más detalles en la tabla a continuación, ya que la profundidad de la aguja debe ajustarse a la indicación y al perfil de seguridad.
| Profundidad de la aguja (aprox.) | Indicación típica | Respuesta esperada del colágeno |
|---|---|---|
| 0,25–0,5 mm | Problemas epidérmicos, absorción del producto. | Estimulación mínima del colágeno dérmico; penetración tópica mejorada |
| 0,5–1,0 mm | Líneas finas, cicatrices superficiales. | Activación moderada de fibroblastos y deposición de colágeno |
| 1,0–2,5 mm | Cicatrices profundas de acné, laxitud. | Lesión dérmica robusta con estimulación de colágeno más fuerte; más tiempo de inactividad |
| >2,5 mm (raro) | Procedimientos especializados | Riesgo mayor; inducción significativa de colágeno pero requiere experiencia |
Advierto que aumentar la profundidad suele producir un mayor estímulo de colágeno, pero también aumenta el riesgo y el tiempo de recuperación. Insisto en que la elección de la profundidad debe basarse en el criterio profesional.
Número de pases, tipo de dispositivo y técnica
La energía total administrada (combinación de profundidad de la aguja, número de pasadas y cadencia) afecta la respuesta del colágeno. Indico que las técnicas consistentes y controladas, realizadas por profesionales capacitados, producen resultados más reproducibles que los tratamientos agresivos y sin control.
Frecuencia de tratamiento y sesiones acumuladas
La síntesis de colágeno es acumulativa; múltiples tratamientos, espaciados adecuadamente, suelen producir mejores resultados. Suelo recomendar una serie de tres a seis tratamientos con intervalos de cuatro a seis semanas para diversas indicaciones, adaptando el plan a la respuesta individual.
Terapias complementarias y tratamientos combinados
El uso de factores de crecimiento, plasma rico en plaquetas (PRP), vitamina C tópica o láseres, junto con la microaguja, puede aumentar la producción de colágeno. Advierto que las estrategias combinadas deben basarse en la evidencia y administrarse en el momento adecuado para evitar la sobreestimulación o un mayor riesgo de efectos adversos.
Estilo de vida y salud sistémica
La nutrición, el tabaquismo, la exposición solar, el sueño y las afecciones sistémicas (p. ej., diabetes, enfermedades autoinmunes) influyen en la cicatrización de heridas y la síntesis de colágeno. Constantemente les aconsejo a mis pacientes que optimizar la salud sistémica mejora los resultados y acorta la recuperación.
Evidencia clínica: qué muestran los ensayos sobre el momento de los cambios de colágeno
Resumiré los hallazgos clave de estudios publicados para que los lectores puedan ver cómo la investigación controlada se alinea con la experiencia clínica. Hago hincapié tanto en los criterios de valoración histológicos como en los clínicos.
Hallazgos histológicos de estudios representativos
Varios estudios histológicos demuestran un aumento en la deposición de colágeno incluso 4 semanas después del tratamiento, con formas de colágeno más pronunciadas y maduras a las 12 semanas. Observo que las biopsias suelen mostrar un aumento en el contenido de colágeno, la proliferación de fibroblastos y la neovascularización en estos momentos.
Resultados clínicos y plazos informados por los pacientes
Los estudios clínicos suelen reportar mejoras notables en la textura y la cicatrización en un plazo de 1 a 3 meses, con mejoras continuas hasta por 6 meses. Cabe destacar que la satisfacción del paciente suele estar relacionada con el número acumulado de sesiones y un asesoramiento preoperatorio realista.
Monitoreo del crecimiento de colágeno: medidas objetivas y subjetivas
Recomiendo una combinación de mediciones objetivas y resultados informados por los pacientes para evaluar el progreso. Explico métodos prácticos que tanto médicos como pacientes pueden usar para monitorear los cambios.
Herramientas de imagen y biofísicas
El ultrasonido de alta frecuencia, la tomografía de coherencia óptica (OCT) y las mediciones con cutómetro permiten cuantificar el aumento del grosor y la elasticidad dérmica. Advierto que, si bien estas herramientas son útiles en la investigación y en clínicas especializadas, es posible que no estén disponibles en todas las consultas.
Escalas estandarizadas de fotografía y calificación clínica
La fotografía estandarizada con iluminación, ángulos y posiciones consistentes es una forma fiable de documentar mejoras visibles. Suelo utilizar escalas validadas de clasificación de cicatrices y arrugas para ofrecer comparaciones objetivas en diferentes momentos.
Resultados informados por el paciente y evaluación táctil
La percepción del paciente sobre la textura, la firmeza y la confianza son resultados importantes que, en ocasiones, preceden a cambios estructurales mensurables. Incluyo la evaluación táctil de la firmeza de la piel y la palpación como evaluaciones prácticas en la consulta que complementan las imágenes.
Dispositivos de microagujas para uso doméstico frente a tratamientos profesionales
Compararé la estimulación y la seguridad de los rodillos y bolígrafos dérmicos caseros con los procedimientos profesionales en la consulta. Recomiendo prácticas basadas en la evidencia para lograr resultados sin riesgos innecesarios.
Profundidad comparativa y estimulación del colágeno
Los dispositivos domésticos suelen utilizar agujas cortas (0,2-0,5 mm) que mejoran principalmente la absorción tópica y producen una inducción mínima de colágeno dérmico. Cabe destacar que los tratamientos profesionales con agujas más profundas (1,0 mm o más) generan una lesión dérmica controlada y un estímulo más potente para la síntesis de colágeno.
Seguridad, esterilidad y riesgo de complicaciones
Los tratamientos profesionales reducen el riesgo de infección y garantizan la selección de la técnica y la profundidad adecuadas. Advierto que el uso inadecuado del dispositivo en casa puede causar infección, hiperpigmentación postinflamatoria o cicatrices en personas susceptibles.
Optimización de la microaguja para maximizar el crecimiento del colágeno
Recomendaré medidas prácticas antes, durante y después del tratamiento que mejoran la producción de colágeno y minimizan las complicaciones. Enfatizo que la adherencia al protocolo y la planificación individualizada son fundamentales.
Optimización del pretratamiento
Recomiendo suspender los retinoides y ciertos exfoliantes según las indicaciones del profesional, y controlar el acné activo o las infecciones antes del procedimiento. También recomiendo que dejar de fumar y mejorar la nutrición en las semanas previas al tratamiento puede acelerar la cicatrización.
Consideraciones durante el procedimiento
Recalco la importancia de una anestesia, una selección de la profundidad y una técnica adecuadas para garantizar la creación consistente de microcanales sin sobretraumatizar el tejido. También recomiendo utilizar una técnica estéril y dispositivos de alta calidad para minimizar las complicaciones.
Cuidados postratamiento para favorecer la formación de colágeno.
Después del procedimiento, recomiendo una limpieza suave, protección solar y un soporte tópico adecuado, como sérums con factores de crecimiento o ácido hialurónico. Normalmente, pospongo la introducción de retinoides y principios activos agresivos hasta que la epidermis se haya reepitelizado para evitar la irritación y la interrupción de la cicatrización.
Agentes tópicos e inyectables que mejoran la respuesta del colágeno.
Cubriré los complementos con evidencia de acción sinérgica y brindaré consideraciones de tiempo para maximizar el beneficio.
Plasma rico en plaquetas (PRP)
El PRP contiene factores de crecimiento concentrados que, al aplicarse durante o inmediatamente después de la microaguja, pueden aumentar la actividad de los fibroblastos. Observo que estudios aleatorizados muestran mejores resultados clínicos cuando se combina el PRP con la microaguja en comparación con la microaguja sola.
Sueros y péptidos de factores de crecimiento
Los péptidos tópicos y los sueros con factores de crecimiento pueden favorecer la producción de matriz durante la fase proliferativa. Advierto que la penetración depende del momento del cierre de los microcanales y del tamaño molecular de los principios activos.
Vitamina C y antioxidantes tópicos
El ácido ascórbico es un cofactor para la reticulación del colágeno y puede favorecer su maduración. Recomiendo introducir sueros de vitamina C después de la cicatrización de la epidermis para minimizar la irritación y maximizar la protección antioxidante.
Retinoides y momento oportuno
Los retinoides son potentes estimuladores de la remodelación dérmica, pero pueden ser irritantes si se aplican demasiado pronto. Recomiendo esperar hasta que la reepitelización esté completa (normalmente de 7 a 14 días) antes de reanudar el tratamiento con retinoides, con una reintroducción gradual.
Seguridad, efectos secundarios y cómo afectan los resultados del colágeno.
Priorizaré la seguridad y describiré los efectos secundarios comunes, la mitigación de riesgos y cómo las complicaciones pueden retrasar o afectar la formación de colágeno.
Efectos secundarios comunes y curación esperada
Es normal que se presente enrojecimiento, hinchazón y pequeñas costras temporales, lo cual no indica un mal pronóstico. Explico que estas reacciones forman parte de la cicatrización normal y deberían desaparecer sin intervención en la mayoría de los casos.
Infección, hiperpigmentación y cicatrices.
En raras ocasiones, puede producirse infección, hiperpigmentación postinflamatoria (HPI) o cicatrización hipertrófica, lo que puede afectar la estructura del colágeno. Recomiendo la detección y el tratamiento tempranos (antibióticos tópicos, control de la pigmentación o derivación para el tratamiento de cicatrices) para preservar los resultados a largo plazo.
Preocupaciones y contraindicaciones autoinmunes
Los pacientes con ciertos trastornos autoinmunes, infecciones cutáneas activas o tendencia a la formación de queloides requieren una evaluación cuidadosa. De forma rutinaria, busco contraindicaciones y ajusto o evito la microaguja cuando el riesgo supera el beneficio.
Gestión de expectativas y planificación del tratamiento
Brindaré orientación sobre objetivos realistas y cómo diseñar un plan de tratamiento que se alinee con los resultados y plazos deseados.
Establecer plazos realistas
Comunico claramente que las mejoras significativas impulsadas por el colágeno suelen aparecer en un plazo de 1 a 3 meses y alcanzan su punto máximo alrededor de los 3 a 6 meses. Siempre comento que a menudo se necesitan varias sesiones y que la remodelación final continúa durante muchos meses.
Planes de tratamiento individualizados
Treatment frequency, needle depth, and adjunctive therapies should be tailored to the individual’s anatomy, goals, and tolerance. I prefer to set incremental goals and reassess after each session to refine the plan.
Practical patient checklist: before and after treatment
I provide a brief checklist that I give patients to maximize safety and outcomes. This list is meant to be a practical, at-a-glance guide.
- Pre-treatment: Stop retinoids 3–7 days before (depending on strength), control active acne, avoid sunburn, maintain hydration, and discuss medications.
- Day of treatment: Arrange transportation if sedation is used, expect redness and swelling, and plan minimal social activities for 24–48 hours.
- Post-treatment: Use gentle cleanser, avoid makeup for 24 hours or as directed, apply sunscreen diligently, and delay potent actives until cleared by your provider.
- Long-term: Follow the recommended treatment series, avoid smoking, maintain sun protection, and schedule follow-ups.
Frequently asked questions (FAQ)
I will answer common patient queries succinctly to reduce uncertainty and facilitate informed consent.
When will I personally notice a difference?
Most patients I treat report subtle improvements within 4–8 weeks and more marked changes by 3 months. Final results often continue to improve up to six months after the last treatment.
Is more aggressive treatment always better for collagen growth?
No. I caution that more aggressive depth or excessive passes increase risk without guaranteeing proportionally better outcomes. The optimal treatment balances efficacy with safety and is individualized.
Can I combine microneedling with other cosmetic procedures?
Yes, combining with PRP, lasers, or fillers can be effective when sequenced properly. I recommend spacing procedures appropriately and discussing an integrated plan with your provider.
How many sessions will I need?
A typical starter series is three treatments spaced 4–6 weeks apart, but the total number depends on the indication and response. I personally reassess after each session and adapt the plan based on observed progress.
Case examples: practical timelines from my clinical practice
I will describe representative cases to illustrate realistic timelines and outcomes that reflect what I see in practice.
Case 1: Mild photoaging, 45-year-old woman
I treated a 45-year-old patient with three sessions at 4-week intervals using 1.0 mm depth for cheeks. She reported subtle texture improvement at 6 weeks and substantial tightening and reduced fine lines at 3 months, with continued improvement through month 6.
Case 2: Atrophic acne scarring, 30-year-old man
I used 1.5–2.0 mm depths for targeted scar remodeling over five sessions spaced 6 weeks apart. Early collagen deposition was apparent clinically at 8–12 weeks, with notable scar softening and volume restoration at 4–6 months.
Final recommendations for clinicians and patients
I will summarize practical, evidence-based recommendations so you can apply them confidently.
- Counsel patients that collagen growth is a biological process that takes time; expect progressive improvement rather than instant change.
- Tailor needle depth, session frequency, and adjunctive therapies to the clinical indication and patient factors.
- Use objective monitoring when possible, and combine with standardized photography for documentation.
- Prioritize safety: sterile technique, appropriate patient selection, and conservative escalation of treatment intensity.
Conclusión
I hope this detailed overview clarifies when microneedling results begin to show collagen growth and how the process evolves over time. I encourage patients and clinicians to set realistic timelines, to monitor progress methodically, and to use evidence-based adjuncts to maximize outcomes while maintaining safety.