? How can I systematically prevent infections after microneedling and keep my patients safe while optimizing outcomes?
Introduction
I present a comprehensive infection prevention protocol for post-microneedling care that synthesizes clinical best practices, practical workflow steps, and patient education strategies. I wrote this protocol to be actionable for clinicians who perform microneedling or for clinical managers who are responsible for infection-control policies. My goal is to reduce infectious complications, improve wound-healing outcomes, and make post-procedure instructions clear and reproducible.
Why infection prevention matters after microneedling
I understand that microneedling intentionally creates controlled micro-injuries in the skin to stimulate remodeling. Those microchannels transiently bypass the epidermal barrier, which increases the theoretical and real risk of bacterial, viral, and fungal invasion. Preventing infection is essential not only to avoid acute complications but also to prevent scarring, pigmentary changes, and treatment interruptions.
Brief review of microneedling physiology and infection risk
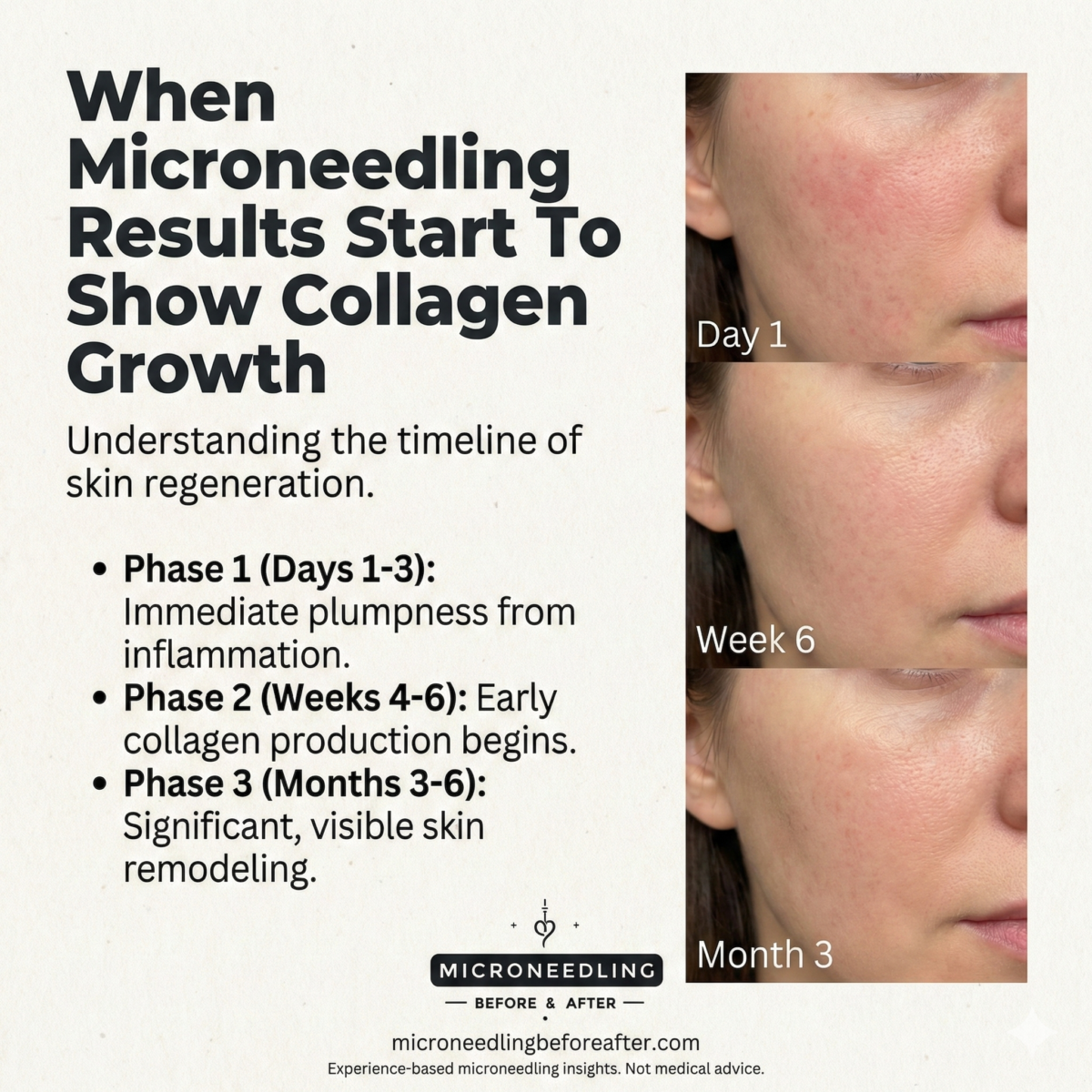
I utilize microneedling to stimulate collagen by creating microchannels that typically close within hours to days depending on needle depth. The depth of injury, skin condition, and adjunctive topical or biologic applications (PRP, serums) influence susceptibility to pathogens. Common organisms implicated post-procedure include Staphylococcus aureus, Streptococcal species, herpes simplex virus (HSV-1), and occasionally atypical mycobacteria following contaminated devices or solutions.
Scope and audience
I wrote this protocol for licensed clinicians (dermatologists, plastic surgeons, aesthetic physicians, nurse practitioners, physician assistants) and clinic staff responsible for peri-procedural care. Sections addressing patient-facing language are written so I can adapt them as printed discharge instructions.
Pre-procedure risk assessment
I begin by assessing patient-specific infection risk factors, procedural factors, and environmental factors.
Patient history and medical screening
I collect a focused history that includes:
- Prior or recurrent HSV infections (cold sores).
- Active skin infections (impetigo, folliculitis, cellulitis) in the treatment area.
- Recent or current use of systemic immunosuppressants, biologics, or high-dose systemic corticosteroids.
- Recent isotretinoin use (within previous 6–12 months) and the timing of past courses.
- Diabetes, uncontrolled glucose, or other comorbidities that impair wound healing.
- Bleeding disorders or anticoagulant therapy that could complicate post-procedure care.
I document these findings and discuss increased risk with the patient when relevant.
Physical exam and skin assessment
I inspect the treatment area for active infections, acneiform lesions, dermatitis, or fresh tattoos. I postpone microneedling over active infection or broken skin. For extensive acne, I consider deferring or treating acne first to minimize bacterial load.
Pre-procedure testing and prophylaxis considerations
I individualize testing and prophylaxis:
- For patients with recurrent HSV, I prescribe antiviral prophylaxis (e.g., acyclovir or valacyclovir) beginning 24 hours before and continuing for 5–7 days after treatment, following local protocols.
- For immunocompromised patients or those with a history of atypical infections, I consult with or refer to a specialist.
- I do not routinely prescribe systemic antibiotics prophylactically for all patients, as evidence does not support universal prophylaxis and overuse promotes resistance. I reserve systemic antibiotics for specific clinical indications or early signs of infection.
Clinic environment and device handling
I maintain a clean, controlled environment and strict device-handling procedures to minimize contamination.
Device and needle management
I use single-use sterile needle cartridges or disposable needle stacks whenever possible. If I use reusable instruments, I ensure validated sterilization via autoclave per manufacturer and local regulatory guidance. I store devices in their sterile packaging until immediately prior to use.
Surface and hand hygiene
I enforce hand hygiene for all staff and use gloves during patient contact. I disinfect procedure surfaces between patients with EPA-registered hospital-grade disinfectants. I minimize clutter and potential fomites in the procedure room.
Aseptic technique for adjunct materials
I treat PRP, growth factors, or serums as potential vectors. I prepare biologic adjuncts in a clean area, use sterile technique, and apply them immediately after preparation. I avoid pooling products or using multi-dose vials without proper aseptic withdrawal.
Procedure technique to minimize infection
I employ procedural steps that reduce contamination and tissue trauma.
Skin preparation
I cleanse the skin thoroughly. I use either chlorhexidine gluconate or povidone-iodine as the pre-procedure antiseptic, allowing the solution to dry fully before needling. I avoid alcohol-based cleansers that may transiently denature epidermal proteins but I do use them judiciously if required by practice standards.
Local anesthesia and topical agents
I use topical anesthetics in single-use tubes or sterile packaging. After anesthetic removal, I re-cleanse the area with an antiseptic prior to needling. I avoid applying non-sterile emollients or makeup prior to the procedure.
Needle depth, passes, and pressure
I select needle depth appropriate for the indication and skin thickness. I avoid overly aggressive settings that create extensive tissue damage beyond therapeutic intent. I control the number of passes and maintain consistent technique to prevent excessive trauma that can predispose to infection.
Adjuncts (PRP, serums)
When applying PRP or other biological adjuncts, I confirm sterility. I apply adjuncts with sterile instruments and avoid contact between stocked product and non-sterile surfaces.
Immediate post-procedure care (first 0–24 hours)
I give precise verbal and written instructions, and I summarize key points verbally at discharge.
Immediate cleaning and dressing
I wipe the treated area with sterile normal saline or sterile saline-soaked gauze. I may apply a thin layer of a sterile, non-comedogenic emollient or a physician-recommended post-procedure balm in a single-use tube to reduce transepidermal water loss and provide a temporary barrier. I avoid ointments that can trap bacteria unless specifically indicated.
I advise patients to avoid occlusive dressings unless instructed, because occlusion can increase humidity and bacterial growth. If I use an occlusive dressing (rarely), I provide clear removal instructions and a timeline.
Activity and exposure restrictions
I advise patients to:
- Avoid touching their face with unwashed hands.
- Not apply makeup for at least 24 hours (or per product-specific guidance).
- Avoid hot baths, saunas, pools, and hot tubs for 72 hours to reduce exposure to waterborne pathogens.
- Avoid heavy exercise for 24–48 hours to limit perspiration and bacterial transfer.
Pain control
I recommend acetaminophen or short-duration NSAIDs unless contraindicated. I avoid recommending aspirin for patients at bleeding risk unless indicated.
Post-procedure timeline and detailed care instructions
The following timeline breaks down care into clear phases so patients know what to expect and when to seek help.
0–24 hours: initial epithelial response
The treated skin is typically erythematous and may be edematous. I instruct gentle cleansing with sterile saline or a mild non-irritating cleanser twice daily. I recommend applying the prescribed post-procedure balm or a sterile, fragrance-free moisturizer as directed. I discourage exfoliants, retinoids, or alcohol-based toners.
24–72 hours: barrier recovery and re-epithelialization
Microchannels begin to close during this period. I encourage continued gentle hygiene, avoidance of makeup until clinically appropriate, and ongoing avoidance of pools, hot tubs, and heavy sweating. I reinforce antiviral prophylaxis adherence if indicated.
3–7 days: continued healing and possible mild peeling
I expect gradual reduction in erythema and occasional mild scaling. I recommend broad-spectrum sunscreen (SPF 30 or greater) when outdoors and physical blockers if skin is sensitive. I advise avoiding topical active agents (retinoids, chemical exfoliants, strong vitamin C) until full re-epithelialization.
>7 days: resumption of normal skincare
I allow reintroduction of active skincare ingredients once the epidermis has fully healed and there is no crusting or open areas. If combining with other procedures (e.g., laser), I ensure a safe interval based on tissue recovery and risk.
Table: Clear post-procedure patient instructions (concise handout)
| Timeframe | Action I instruct | Products to use | Activities to avoid |
|---|---|---|---|
| Immediately (0–24h) | Rinse gently with sterile saline/cleanser; apply thin layer of prescribed balm 2–3x/day | Sterile saline; single-use balm tube (physician-recommended) | Makeup, touching face, hot showers, pools, saunas |
| 24–72h | Continue gentle cleansing and moisturizing; monitor for increased pain/redness | Fragrance-free moisturizer; antiviral (if prescribed) | Heavy exercise, prolonged sun exposure, swimming |
| 3–7 days | Expect peeling; begin gentle sunscreen application when outdoors | Physical sunscreen (zinc oxide), gentle cleanser | Retinoids, chemical peels, aggressive exfoliation |
| >7 days | Resume normal skincare if fully healed; contact clinic if delayed healing | Resume chosen products after clinician approval | Proceed with other procedures only after clinician clearance |
Recognizing infection: signs, differential diagnosis, and early action
I emphasize early recognition to enable prompt treatment.
Clinical signs of infection
I teach patients to seek immediate care for:
- Increasing localized pain beyond expected discomfort.
- Increasing erythema that spreads rather than fades.
- New purulent drainage or yellow-green crusting.
- Fever, chills, or systemic symptoms.
- Development of vesicles or grouped lesions suggestive of HSV.
Common mimics and differentiators
I differentiate between normal inflammatory responses and infection:
- Post-procedure erythema typically peaks early and then improves.
- Sterile pustules or transient papules from occlusion or product reaction can mimic infection but are usually non-tender and non-progressive.
- HSV presents early with grouped vesicles and may be associated with prodrome (tingling, burning).
When in doubt, I perform clinical assessment and, if necessary, culture drainage or swab lesions for bacterial or viral PCR testing.
Management of suspected infection
I individualize treatment based on presentation, organism likelihood, and patient factors.
Mild localized bacterial infection
I may start an empiric oral antibiotic targeting common skin pathogens (e.g., dicloxacillin, cephalexin) while awaiting culture results, adjusting therapy per sensitivity. I consider topical antibiotics (e.g., mupirocin) for focal superficial infections in combination with oral therapy if indicated.
Severe or spreading infection
I arrange urgent evaluation and may start broad-spectrum antibiotics, arrange wound care, and consider hospitalization if systemic involvement or rapid progression occurs.
Herpetic infections
I initiate antiviral therapy (e.g., valacyclovir) promptly when HSV is suspected. I counsel regarding potential scarring and the need for therapy even if the patient had no prior diagnosed herpes history, because microneedling can trigger primary or recurrent episodes.
Atypical mycobacterial or fungal infections
I suspect atypical mycobacteria or fungal pathogens with delayed presentations (weeks), nodular or draining lesions, or lack of response to standard antibiotics. I obtain cultures, perform acid-fast bacilli tests, and refer to infectious disease as appropriate.
Antibiotic stewardship and documentation
I avoid reflexive empiric antibiotics without clinical indication. I document clinical findings, decision rationale, cultures obtained, and patient education in the medical record. I follow local antibiogram patterns when selecting empiric therapy.
Special situations
Combined procedures (PRP, platelet-rich fibrin, lasers)
When combining microneedling with PRP or lasers, I increase vigilance for sterility and may modify post-procedure instructions, including longer avoidance of water immersion and stricter wound care. I ensure that the interval between microneedling and other resurfacing procedures is safe and evidence-based.
Immunocompromised patients
I approach immunocompromised patients with heightened caution. I consider consultation and may defer elective microneedling. If proceeding, I use strict asepsis, consider prophylactic antivirals if indicated, and provide closer follow-up.
Pregnant or breastfeeding patients
I evaluate the risk-benefit profile. I may defer aesthetic microneedling in pregnancy unless clinically indicated. If treatment proceeds, I avoid products with contraindicated agents and document informed consent.
Home microneedling and consumer devices
I discourage or set strict limitations on at-home microneedling for devices that breach the dermal barrier (needle lengths >0.25 mm). I educate patients on the higher infection risks from non-sterile at-home use and advise professional treatments as safer alternatives. If a patient will use a home device, I provide detailed cleaning and single-user instructions.
Patient education and written consent
I obtain informed consent that includes explicit discussion of infection risk, expected course, signs of complications, and contact information for urgent concerns. I provide a printed or electronic discharge sheet summarizing key dos and don’ts and when to call.
Table: Clinic checklist for infection prevention (for clinician use)
| Task | Performed (Y/N) | Notes |
|---|---|---|
| Pre-procedure infection screen documented | ||
| Antiviral prophylaxis given when indicated | ||
| Single-use sterile needle cartridge prepared | ||
| Skin antiseptic applied and dried | ||
| PRP/serum prepared aseptically | ||
| Post-procedure instructions provided and documented | ||
| Follow-up appointment scheduled (or patient advised when) |
Follow-up plan and escalation pathway
I schedule follow-up contact within 48–72 hours (phone or telemedicine) for higher-risk patients or those who received deep treatments or biologic adjuncts. I advise in-person assessment for any concerning symptoms. I maintain low threshold for culture, blood tests, and specialty referral if an atypical course develops.
Quality improvement and morbidity tracking
I track adverse events, infection rates, and procedural complications. I review cases in morbidity and mortality or quality improvement meetings to refine protocols. I audit sterilization logs, device handling, and staff training regularly.
Legal, regulatory, and billing considerations
I align my protocols with local regulatory guidance regarding device sterilization, product labeling, and practice scope. I document informed consent and clinical indications to support medico-legal defensibility. I code and bill appropriately for time and services associated with complications or post-procedure care.
Practical examples and scenarios
I include a few clinical scenarios to illustrate how I apply the protocol.
Scenario 1: Patient with history of recurrent cold sores
I prescribe valacyclovir 500 mg orally twice daily, starting 24 hours before treatment and continuing for 5 days after. I document counseling and verify adherence at follow-up.
Scenario 2: Early localized cellulitis 4 days post-procedure
I assess the area, obtain a wound swab for culture, and start an empiric oral antibiotic covering Staphylococcus and Streptococcus while awaiting results. I arrange in-person follow-up within 48 hours.
Scenario 3: Delayed nodular lesions after combined microneedling and PRP
I suspect atypical mycobacterial infection, obtain tissue biopsy and cultures including AFB, and refer to infectious disease for prolonged combination therapy based on sensitivity testing.
Recommendations for product selection
I recommend products with clear sterility and single-use packaging. Below is a concise table of product guidance.
Table: Products I recommend and those I advise to avoid
| Recommended | Avoid or use with caution |
|---|---|
| Single-use sterile needle cartridges | Multi-use cartridge reuse without sterilization |
| Single-use anesthetic tubes or sterile packaging | Community jars or unsealed tubes |
| Sterile saline for immediate cleansing | Tap water irrigation for initial wound care |
| EPA-registered surface disinfectants | Inadequate disinfectants or unverified home remedies |
| Physician-grade, sterile PRP prepared aseptically | Unknown-source serums or multi-dose vials opened in non-sterile environment |
Training and staff competence
I ensure staff receive competency-based training in aseptic technique, device setup, patient screening, recognition of complications, and post-procedure instruction delivery. I maintain training records and perform periodic competency reassessments.
Documentation templates and sample patient handout
I use concise templates to standardize documentation: pre-procedure risk assessment, informed consent with infection-risk language, sterile device lot numbers, and discharge instructions. A sample patient handout includes the short timeline and clear red flags, and I give a copy at discharge.
Limitations and clinical judgment
I acknowledge that recommendations must be adapted to local epidemiology, regulatory constraints, individual patient factors, and evolving evidence. I base decisions on current best practices while being ready to modify the protocol as new data emerge.
Summary and key takeaways
I summarize the core principles:
- Screen patients for infection risk and defer treatment when indicated.
- Use single-use sterile needles or validated sterilization for reusable devices.
- Employ antiseptic skin prep and aseptic technique for products and adjuncts.
- Provide clear, written post-procedure instructions with a timeline.
- Recognize early signs of infection and act promptly with appropriate cultures and targeted therapy.
- Maintain thorough documentation, staff training, and quality monitoring.
I consider infection prevention after microneedling a combination of procedure planning, meticulous technique, patient education, and timely management of complications. Implementing a structured protocol reduces infection rates, improves patient satisfaction, and protects both patients and clinicians.
Disclaimer
I provide this protocol as an informational resource and not a substitute for individualized medical judgment. I advise clinicians to apply local regulations and consult infectious disease or dermatology colleagues for complicated cases. If you want, I can draft printable patient discharge instructions, a clinic poster for staff steps, or an editable checklist tailored to your practice.