? Have you ever wondered whether microneedling is safe for everyone, or if there are situations where I would advise against it?
Who Should Not Do Microneedling
Microneedling is a popular skin procedure that I often discuss with patients and friends. It can improve texture, scars, fine lines, and product absorption, but it isn’t suitable for everyone. In this article I’ll walk you through the main groups of people who should avoid microneedling, explain why, and offer safe alternatives or timing recommendations where appropriate. I’ll also cover practical steps I recommend before pursuing microneedling so you can make an informed decision with your clinician.
What microneedling does and why contraindications matter
Microneedling uses tiny needles to create controlled micro-injuries in the skin. Those micro-injuries trigger a healing response that stimulates collagen and elastin production. While that process can be beneficial, it also involves deliberately breaking the skin’s barrier. When I consider whether a person is a candidate, I always weigh healing capacity, infection risk, scarring tendency, medications, and any condition that could be worsened by trauma or impaired healing.
I’ll be specific: some conditions make microneedling risky because they increase infection risk, delay healing, or raise the chance of abnormal scarring or pigmentation. In other cases, underlying therapies or treatments can interact with microneedling. I find it helpful to break the contraindications down by category.
Absolute and relative contraindications — how I think about them
I separate contraindications into absolute (I would not proceed) and relative (I might proceed only after addressing or modifying the issue). Absolute contraindications are conditions or situations where microneedling should be avoided until the problem is resolved. Relative contraindications mean microneedling may be possible, but only after careful assessment, treatment, or waiting periods.
Below I’ll list specific conditions, explain the reasons, and give my practical recommendations.
Active skin infections (bacterial, fungal, viral)
If you have an active skin infection in the treatment area—such as impetigo, cellulitis, active tinea (fungal infection), or an active herpes simplex outbreak—I would not perform microneedling.
I explain this to patients like this: creating microchannels in infected skin allows microbes to spread deeper into the tissue and into the bloodstream. That raises the chance of a serious infection.
What I recommend: treat the infection first and wait until it’s fully resolved. For herpes simplex (cold sores), many clinicians give antiviral prophylaxis and postpone treatment until healing or starting antivirals; I prefer waiting until there is no active lesion and discussing prophylaxis if you have a history of frequent outbreaks.
Active inflammatory acne, rosacea flare-ups, psoriasis, eczema
If you have active inflammatory acne (red, pustular, or cystic lesions), an active rosacea flare, psoriasis plaques, or atopic dermatitis (eczema) in the area, I would advise against microneedling at that time.
Why? Microneedling can spread bacteria and inflammatory mediators, potentially worsening acne and causing more irritation or post-procedure complications. With psoriasis or eczema, the trauma could trigger flares or Koebner phenomenon (new lesions forming at sites of injury).
What I recommend: treat the active condition first until it is under control. For acne, that might mean topical or oral medications and waiting a few months if you recently started systemic therapy. For rosacea and inflammatory dermatoses, achieve stability for several weeks before considering microneedling.
History of keloids or hypertrophic scarring
If you have a personal or strong family history of keloid formation or hypertrophic scars, I generally advise against microneedling.
I say this because any procedure that intentionally injures the skin can trigger overactive scar formation in predisposed individuals. While microneedling is sometimes promoted as a scar treatment, people prone to keloids are at higher risk of worsening scarring.
What I recommend: avoid microneedling over areas that have developed keloids in the past. If scar treatment is needed, I suggest consulting a dermatologist or plastic surgeon for safer options such as steroid injections, silicone therapy, or other controlled modalities.
Systemic isotretinoin (Accutane) use — recent or ongoing
If you’re on systemic isotretinoin (commonly known as Accutane) or completed it recently, I take a conservative approach. Historically many clinicians recommended waiting 6 to 12 months after finishing isotretinoin before performing microneedling or other resurfacing procedures.
Why? Isotretinoin can impair wound healing and increase the risk of scarring with invasive procedures, though recent evidence is mixed. Still, I prefer to be cautious.
What I recommend: if you’re currently on isotretinoin, avoid microneedling. If you finished isotretinoin, discuss timing with your prescriber—most often I would wait at least 6 months, sometimes up to 12 months, depending on dose and healing history.
Blood clotting disorders and anticoagulant therapy
If you have a bleeding disorder (for example, hemophilia) or you’re taking anticoagulants (blood thinners) such as warfarin, direct oral anticoagulants, or high-dose aspirin, microneedling carries higher bleeding and bruising risk.
I emphasize safety: increased bleeding can complicate the procedure, affect outcomes, and prolong healing.
What I recommend: consult both your prescribing physician and the clinician performing the procedure. In some situations, temporary medication adjustments are possible; in others, microneedling may be contraindicated. At minimum, I’d expect enhanced consent and a strategy to minimize bleeding.
Immunosuppression and active cancer treatment
If you are immunosuppressed (for example, taking systemic immunosuppressants, biologics, systemic steroids, chemotherapy) or undergoing active cancer therapy, I would generally avoid microneedling.
My reasoning is that immunosuppression raises infection risk and may impair wound healing. During active chemotherapy or immunosuppressive therapy, I usually recommend postponing elective skin procedures until immune function improves.
What I recommend: discuss with the treating oncologist or specialist. Postpone elective microneedling until you have clearance and your immune system has recovered.
Uncontrolled diabetes
If you have poorly controlled diabetes, I am cautious about microneedling because impaired glucose control can delay healing and increase infection risk.
I don’t want to risk complications, so I prefer that systemic disease be stable and well-managed before elective skin procedures.
What I recommend: achieve good glycemic control and get sign-off from your primary care provider or endocrinologist prior to treatment.
Active or recent skin cancer in the treatment area
If you have an active skin cancer in the area you want treated, or are recovering from recent skin cancer treatment, microneedling is not appropriate until the clinician caring for your cancer confirms it’s safe.
I always prioritize cancer management. Microneedling could interfere with surveillance and healing after excision or radiation.
What I recommend: wait until your skin cancer has been treated and you have clear guidance from your dermatologist or oncologist.
Recent chemical peel, laser resurfacing, or other ablative procedures
If you’ve recently had an aggressive chemical peel, laser resurfacing, or another ablative procedure, I advise waiting until the skin has fully healed before microneedling.
I explain that combining or spacing procedures improperly can cause cumulative trauma, increasing scarring and pigmentary problems.
What I recommend: discuss the timeline with the clinician who performed the previous procedure. Typical intervals vary but often range from several weeks to months depending on the intensity of the prior treatment.
Pregnancy and breastfeeding
If you’re pregnant or breastfeeding, I generally recommend avoiding microneedling as an elective procedure.
My reasoning: there’s limited evidence about the safety of microneedling in pregnancy, and pregnancy-related hormonal changes can affect healing and pigmentation. Additionally, topical agents sometimes used with microneedling (like retinoids) are contraindicated in pregnancy.
What I recommend: postpone microneedling until after pregnancy and breastfeeding, or consult both your obstetrician and dermatologist if there are special circumstances.
Recent facial fillers, threads, or implants
If you’ve recently had dermal fillers, thread lifts, or other implants in the treatment area, timing matters. Microneedling too close to filler injections can increase the risk of infection and product displacement.
I typically advise waiting a period after filler placement and being cautious near filler sites.
What I recommend: for most hyaluronic acid fillers, I suggest waiting at least 2 weeks and often longer, with some clinicians preferring 4 weeks. For permanent implants or threads, discuss with the treating provider about safe timing.
Tattoos and permanent makeup
Microneedling directly over tattoos or permanent makeup can alter pigment, cause pigment migration, and increase infection risk.
I usually tell people to avoid microneedling directly over tattoos, unless a specialist with experience is planning the procedure for a specific reason.
What I recommend: treat only non-tattooed skin or consult a specialist experienced in working with tattooed areas.
Known allergies to numbing agents or topical ingredients
If you have a documented allergy to topical anesthetics or to ingredients commonly used in post-care protocols (like certain antiseptics or topical antibiotics), I will consider that a contraindication until we find alternatives.
I always ask about allergies because reactions during or after the procedure can complicate healing.
What I recommend: disclose all allergies and prior reactions. We can often choose alternative products, but this may affect scheduling or the decision to proceed.
Recent viral infections or systemic illness
If you’re currently ill with a systemic infection (for example, flu-like illness or COVID-19) I would postpone microneedling until you’ve recovered.
I emphasize rest and recovery first; the body heals best when not fighting another active illness.
What I recommend: reschedule after full recovery and ensure no active fevers or systemic symptoms.
Table: Quick reference for common contraindications
I find tables useful for quick clinical decision-making. Below is a concise summary of common contraindications, why they matter, and what I typically recommend.
| Condition / Situation | Why it’s a concern | My practical recommendation |
|---|---|---|
| Active skin infection (bacterial/fungal/herpetic) | Risk of deeper infection, spread | Treat infection, wait until resolved |
| Active inflammatory acne, rosacea, psoriasis, eczema | Can worsen inflammation or trigger lesions | Control condition first; reassess when stable |
| History of keloids/hypertrophic scarring | Risk of abnormal scarring | Avoid microneedling over prone areas; consider alternatives |
| Systemic isotretinoin (current/recent) | Impaired healing; scarring risk | Avoid during therapy; wait 6–12 months after completion |
| Anticoagulant therapy / bleeding disorders | Excess bleeding, bruising, hematoma | Consult prescribing doctor; may postpone or adjust meds |
| Immunosuppression / chemo | Impaired healing, infection risk | Postpone until immune recovery; get clearance |
| Uncontrolled diabetes | Poor healing, infection | Achieve glycemic control; get medical clearance |
| Active skin cancer or recent excision | Interferes with cancer care | Wait until cleared by specialist |
| Recent ablative treatments (laser/peel) | Cumulative trauma, delayed healing | Follow clinician’s recommended interval |
| Pregnancy / breastfeeding | Limited safety data; topical contraindications | Postpone until after pregnancy/breastfeeding |
| Recent fillers, threads, implants | Infection risk, filler displacement | Wait recommended interval; consult treating provider |
| Tattoos/permanent makeup | Pigment alteration, infection | Avoid direct treatment; consult specialist |
| Allergies to topical agents/anesthetics | Risk of allergic reaction | Use alternatives or postpone |
Special considerations: melasma, hyperpigmentation, and darker skin types
If you have melasma or darker Fitzpatrick skin types, I proceed cautiously. Microneedling can be helpful for some pigmentary issues, but it can also trigger post-inflammatory hyperpigmentation (PIH) if not done correctly.
I usually recommend a careful pre-treatment regimen (including sun protection and topical agents like hydroquinone or tranexamic acid when appropriate) and conservative settings. In some cases, microneedling combined with cryotherapy or chemical peels is contraindicated for melasma.
What I recommend: see a dermatologist experienced with pigmented skin, follow a pre-treatment plan to stabilize melasma, and use conservative techniques. If melasma is active or unstable, delay treatment.
At-home microneedling devices — extra caution
Home dermarollers and microneedling pens are widely available, but they carry different risks than in-office treatments. I worry about improper sterilization, shared devices, excessive needle length, and aggressive use that increases infection and scarring risks.
I often tell people that in-office procedures are safer due to medical-grade devices, sterile technique, and trained providers.
What I recommend: if you’re considering at-home use, use devices with short needles (typically 0.25 mm) and follow strict hygiene. However, for deeper treatments or if you have any contraindications above, consult a professional instead of DIY.
Medication and topical interactions — what I ask about before treatment
Before I agree to microneedling for anyone, I review medications and topicals that could affect safety:
- Systemic isotretinoin (Accutane): avoid during and for recommended waiting period after.
- Anticoagulants and antiplatelets: assess bleeding risk.
- Systemic immunosuppressants or biologics: discuss risk and timing.
- Topical retinoids and exfoliants: often paused before and after treatment to reduce irritation.
- Oral antibiotics or antivirals: may be used prophylactically in select cases (e.g., cold sore history).
I recommend full disclosure of medications and supplements, including over-the-counter NSAIDs and herbal supplements that affect bleeding (like fish oil, ginkgo, or high-dose vitamin E), so I can advise appropriately.
How I assess candidacy during a consultation
When someone asks me about microneedling, I take a structured approach:
- Medical history: I review systemic diseases, medications, pregnancy status, and autoimmune conditions.
- Dermatologic history: I ask about history of cold sores, acne, keloids, pigmentation concerns, and prior procedures.
- Skin exam: I inspect the treatment area for active lesions, sunburn, or irritation.
- Expectations: I discuss goals, risks, number of sessions, and realistic outcomes.
- Plan: I advise on pre-treatment steps (stop topical retinoids, stabilize disease) and post-care.
I encourage open dialogue because the safest plan depends on individual risk factors.
Alternatives when microneedling is not appropriate
If microneedling is contraindicated, I often suggest safer alternatives depending on the problem you want to treat.
- Superficial chemical peels or gentle light chemical exfoliation — for mild texture and superficial pigmentation, if appropriate.
- Microdermabrasion — noninvasive option for skin texture; lower infection risk.
- Topical medical therapies — retinoids, hydroquinone, tranexamic acid, or prescription creams for pigmentation and texture over time.
- Injectable options — in select cases, fillers or neuromodulators might address volume loss or lines without resurfacing.
- Laser or light therapies — though some lasers share similar contraindications, certain nonablative lasers may be considered when microneedling is inappropriate; always evaluate on a case-by-case basis.
- Scar-specific treatments — for keloids or hypertrophic scars, steroid injections, silicone sheeting, or surgical options with specialized planning.
I always tailor alternatives to the condition and the person’s medical profile.
Safety tips and red flags I use in practice
I give people practical safety advice so they can spot red flags and make informed choices.
- Choose an experienced, licensed provider. I prefer clinicians with medical training or supervised settings.
- Verify the clinic’s sterilization protocols and that single-use, disposable needles are used for in-office treatments.
- Be wary of aggressive pricing or offers that encourage skipping pre-procedure medical review.
- If you notice unusual pain, spreading redness, fever, or pus after treatment, seek urgent medical attention.
- Avoid sun exposure and tanning immediately before and after microneedling to reduce pigmentary complications.
- Follow post-care instructions for cleansers, ointments, and sunscreens strictly—these influence healing and outcomes.
If anything feels “off” during or after the procedure, I urge people to contact their provider promptly.
Frequently asked questions I get from patients
I often get a set of predictable questions. Here are my typical answers:
- Can I get microneedling if I have acne scars? Yes, in many cases microneedling is effective for atrophic acne scars, but not during active inflammatory acne.
- If I’m prone to cold sores, can I still have microneedling? Possibly. I usually recommend antiviral prophylaxis and ensure no active lesions are present.
- Is microneedling safe on all skin tones? Microneedling is generally safer than many lasers for darker skin tones but carries PIH risk; careful technique and pre/post treatments are important.
- Can teenagers have microneedling? I’m cautious with younger skin; if someone is a teen, I assess the underlying issue and often prefer conservative treatments first.
- How many sessions are needed? That depends on the concern; 3–6 sessions spaced weeks apart is common for many indications, but I always tailor the plan.
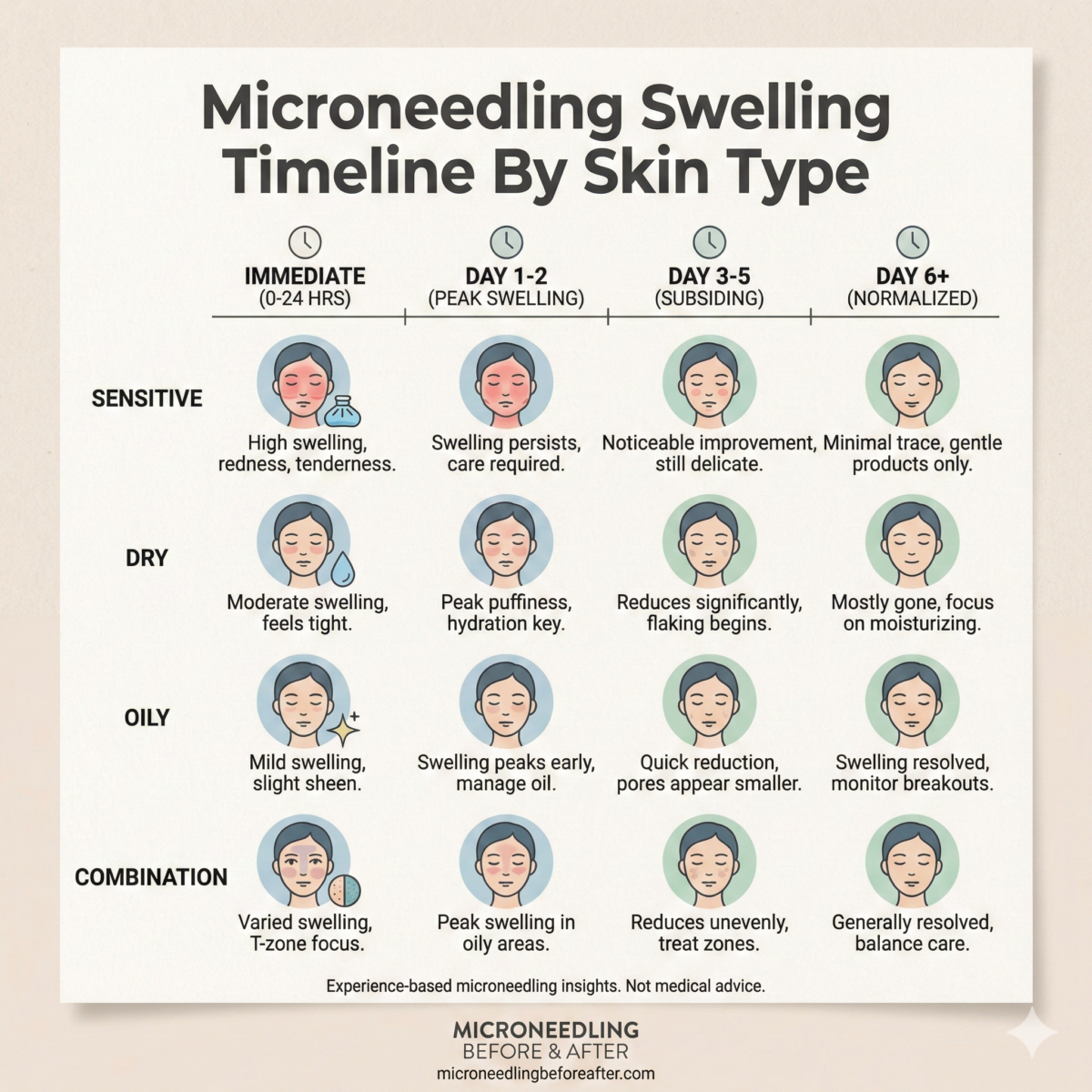
Post-procedure considerations and when to contact a clinician
After microneedling, normal responses include redness, mild swelling, and pinpoint bleeding or bruising that resolves in days. Use gentle cleansers, moisturizers, and sunscreens as instructed.
Contact your clinician if you experience increasing pain, swelling beyond a few days, spreading redness, fever, pus, or if you notice signs of an allergic reaction such as hives or difficulty breathing.
I tell people that prompt attention reduces the risk of complications becoming serious.
Final checklist I use before recommending microneedling
When I’m thinking about whether microneedling is appropriate, I mentally run through this checklist:
- Is the skin free of active infection or inflammatory disease in the area?
- Are there any systemic illnesses or medications that impair healing?
- Is pregnancy or breastfeeding a factor?
- Is there a history of abnormal scarring or bleeding disorders?
- Have recent procedures or treatments been completed in a safe timeframe?
- Is the patient informed about alternatives, risks, and realistic expectations?
If any items raise concern, I postpone or adapt the plan, or I refer to a specialist.
Conclusion
Microneedling can be an effective tool for many skin concerns, but it is not a one-size-fits-all solution. I always evaluate the whole person—medical history, current medications, skin condition, and expectations—before recommending microneedling. There are clear scenarios where I would not perform microneedling or where I would require specific precautions: active infections, uncontrolled systemic conditions, recent isotretinoin use, immunosuppression, pregnancy, and a history of keloids, among others.
If you’re considering microneedling, I encourage you to have a candid conversation with a qualified provider, disclose your full medical history, and follow pre- and post-care instructions closely. When microneedling is avoided for safety reasons, there are typically safer alternatives that can still help you reach your goals without putting your health at risk.
If you want, I can help you think through a specific medical history or concern to determine whether microneedling might be appropriate for you and what timing or alternatives I would suggest.