¿Alguna vez te has preguntado si la microaguja es segura para todos o si hay situaciones en las que no la recomendaría?
¿Quién no debería someterse a la microaguja?
La microaguja es un procedimiento cutáneo popular que suelo comentar con pacientes y amigos. Puede mejorar la textura, las cicatrices, las líneas de expresión y la absorción del producto, pero no es apto para todos. En este artículo, te explicaré los principales grupos de personas que deberían evitar la microaguja, explicaré por qué y ofreceré alternativas seguras o recomendaciones de cuándo aplicarla cuando corresponda. También te explicaré los pasos prácticos que recomiendo antes de someterte a la microaguja para que puedas tomar una decisión informada con tu médico.
Qué hace la microaguja y por qué son importantes las contraindicaciones
La microaguja utiliza agujas diminutas para crear microlesiones controladas en la piel. Estas microlesiones desencadenan una respuesta curativa que estimula la producción de colágeno y elastina. Si bien este proceso puede ser beneficioso, también implica romper deliberadamente la barrera cutánea. Al considerar si una persona es candidata, siempre considero la capacidad de curación, el riesgo de infección, la tendencia a la formación de cicatrices, la medicación y cualquier afección que pueda agravarse por un traumatismo o una cicatrización deficiente.
Seré más específico: algunas afecciones hacen que la microaguja sea riesgosa porque aumenta el riesgo de infección, retrasa la cicatrización o aumenta la probabilidad de cicatrices o pigmentación anormales. En otros casos, las terapias o tratamientos subyacentes pueden interactuar con la microaguja. Me resulta útil desglosar las contraindicaciones por categoría.
Contraindicaciones absolutas y relativas: qué pienso sobre ellas
Clasifico las contraindicaciones en absolutas (no procedería) y relativas (podría proceder solo después de abordar o modificar el problema). Las contraindicaciones absolutas son condiciones o situaciones en las que se debe evitar la microaguja hasta que se resuelva el problema. Las contraindicaciones relativas significan que la microaguja podría ser posible, pero solo después de una evaluación, tratamiento o períodos de espera minuciosos.
A continuación enumeraré condiciones específicas, explicaré las razones y daré mis recomendaciones prácticas.
Infecciones cutáneas activas (bacterianas, fúngicas, virales)
Si tiene una infección cutánea activa en el área de tratamiento (como impétigo, celulitis, tiña activa (infección por hongos) o un brote de herpes simple activo), no realizaría microagujas.
Les explico esto a los pacientes así: la creación de microcanales en la piel infectada permite que los microbios se propaguen más profundamente en el tejido y lleguen al torrente sanguíneo. Esto aumenta el riesgo de una infección grave.
Lo que recomiendo: tratar primero la infección y esperar a que se resuelva por completo. Para el herpes simple (herpes labial), muchos médicos recetan profilaxis antiviral y posponen el tratamiento hasta que se cure o comiencen los antivirales; yo prefiero esperar hasta que no haya una lesión activa y hablar sobre la profilaxis si tiene antecedentes de brotes frecuentes.
Acné inflamatorio activo, brotes de rosácea, psoriasis, eczema.
Si tiene acné inflamatorio activo (lesiones rojas, pustulosas o quísticas), un brote de rosácea activo, placas de psoriasis o dermatitis atópica (eccema) en la zona, le desaconsejaría la microaguja en ese momento.
¿Por qué? La microaguja puede propagar bacterias y mediadores inflamatorios, lo que podría empeorar el acné y causar más irritación o complicaciones posoperatorias. En el caso de la psoriasis o el eccema, el traumatismo podría desencadenar brotes o el fenómeno de Koebner (formación de nuevas lesiones en los puntos de lesión).
Lo que recomiendo: tratar primero la afección activa hasta que esté bajo control. Para el acné, esto podría significar medicamentos tópicos u orales y esperar unos meses si recientemente comenzó una terapia sistémica. Para la rosácea y las dermatosis inflamatorias, es necesario lograr una estabilización durante varias semanas antes de considerar la microaguja.
Historia de queloides o cicatrices hipertróficas
Si tiene antecedentes personales o familiares importantes de formación de queloides o cicatrices hipertróficas, generalmente le aconsejo que no utilice microagujas.
Digo esto porque cualquier procedimiento que dañe intencionalmente la piel puede desencadenar la formación de cicatrices hiperactivas en personas predispuestas. Si bien la microaguja a veces se promociona como un tratamiento para las cicatrices, las personas propensas a los queloides tienen un mayor riesgo de que las cicatrices empeoren.
Recomiendo: evitar la microaguja en zonas con queloides. Si se necesita tratamiento para cicatrices, recomiendo consultar con un dermatólogo o cirujano plástico para opciones más seguras, como inyecciones de esteroides, terapia con silicona u otras modalidades controladas.
Uso sistémico de isotretinoína (Accutane): reciente o continuo
Si está tomando isotretinoína sistémica (comúnmente conocida como Accutane) o la terminó recientemente, adopto un enfoque conservador. Históricamente, muchos médicos recomendaban esperar de 6 a 12 meses después de terminar la isotretinoína antes de realizar microagujas u otros procedimientos de rejuvenecimiento.
¿Por qué? La isotretinoína puede dificultar la cicatrización de heridas y aumentar el riesgo de cicatrices con procedimientos invasivos, aunque la evidencia reciente es contradictoria. Aun así, prefiero ser cauteloso.
Lo que recomiendo: si actualmente toma isotretinoína, evite la microaguja. Si terminó la isotretinoína, consulte con su médico sobre el momento oportuno; normalmente esperaría al menos 6 meses, a veces hasta 12 meses, dependiendo de la dosis y el historial de recuperación.
Trastornos de la coagulación sanguínea y tratamiento anticoagulante
Si tiene un trastorno hemorrágico (por ejemplo, hemofilia) o está tomando anticoagulantes (diluyentes de la sangre) como warfarina, anticoagulantes orales directos o aspirina en dosis altas, la microaguja conlleva un mayor riesgo de sangrado y hematomas.
Hago hincapié en la seguridad: el aumento del sangrado puede complicar el procedimiento, afectar los resultados y prolongar la curación.
Lo que recomiendo: consulte tanto al médico que le recetó el tratamiento como al profesional que realizará el procedimiento. En algunas situaciones, es posible ajustar temporalmente la medicación; en otras, la microaguja podría estar contraindicada. Como mínimo, esperaría un consentimiento informado más amplio y una estrategia para minimizar el sangrado.
Inmunosupresión y tratamiento activo del cáncer
Si está inmunodeprimido (por ejemplo, si toma inmunosupresores sistémicos, productos biológicos, esteroides sistémicos, quimioterapia) o se encuentra bajo terapia activa contra el cáncer, generalmente evitaría la microaguja.
Mi razonamiento es que la inmunosupresión aumenta el riesgo de infección y puede dificultar la cicatrización de heridas. Durante la quimioterapia activa o la terapia inmunosupresora, suelo recomendar posponer los procedimientos cutáneos electivos hasta que mejore la función inmunitaria.
Lo que recomiendo: Consulte con el oncólogo o especialista que lo atiende. Posponga la microaguja electiva hasta que tenga el alta y su sistema inmunitario se haya recuperado.
diabetes no controlada
Si tiene diabetes mal controlada, soy cauteloso con la microaguja porque el control deficiente de la glucosa puede retrasar la curación y aumentar el riesgo de infección.
No quiero correr el riesgo de complicaciones, por lo que prefiero que la enfermedad sistémica esté estable y bien controlada antes de realizar procedimientos electivos en la piel.
Lo que recomiendo: lograr un buen control de la glucemia y obtener la aprobación de su médico de atención primaria o endocrinólogo antes del tratamiento.
Cáncer de piel activo o reciente en el área de tratamiento
Si tiene un cáncer de piel activo en el área que desea tratar, o se está recuperando de un tratamiento reciente contra el cáncer de piel, la microaguja no es apropiada hasta que el médico que atiende su cáncer confirme que es seguro.
Siempre priorizo el tratamiento del cáncer. La microaguja podría interferir con la vigilancia y la cicatrización tras la escisión o la radioterapia.
Lo que recomiendo: esperar hasta que su cáncer de piel haya sido tratado y tenga una guía clara de su dermatólogo u oncólogo.
Peeling químico reciente, rejuvenecimiento con láser u otros procedimientos ablativos
Si recientemente se ha sometido a una exfoliación química agresiva, un rejuvenecimiento con láser u otro procedimiento ablativo, le recomiendo esperar hasta que la piel haya sanado por completo antes de realizar la microaguja.
Explico que combinar o espaciar los procedimientos de forma inadecuada puede causar un trauma acumulativo, aumentando las cicatrices y los problemas pigmentarios.
Lo que recomiendo: Consulte el cronograma con el profesional que realizó el procedimiento anterior. Los intervalos típicos varían, pero suelen oscilar entre varias semanas y meses, dependiendo de la intensidad del tratamiento previo.
Embarazo y lactancia materna
Si está embarazada o amamantando, generalmente recomiendo evitar la microaguja como procedimiento electivo.
Mi razonamiento: existe evidencia limitada sobre la seguridad de la microaguja durante el embarazo, y los cambios hormonales relacionados con el embarazo pueden afectar la cicatrización y la pigmentación. Además, los agentes tópicos que a veces se usan con la microaguja (como los retinoides) están contraindicados durante el embarazo.
Lo que recomiendo: posponer la microaguja hasta después del embarazo y la lactancia, o consultar tanto con su obstetra como con su dermatólogo si hay circunstancias especiales.
Rellenos faciales, hilos o implantes recientes
Si recientemente se ha aplicado rellenos dérmicos, hilos tensores u otros implantes en la zona a tratar, el momento oportuno es importante. La microaguja aplicada demasiado cerca de las inyecciones de relleno puede aumentar el riesgo de infección y desplazamiento del producto.
Generalmente recomiendo esperar un tiempo después de la colocación del relleno y tener cuidado cerca de los sitios de relleno.
Lo que recomiendo: para la mayoría de los rellenos de ácido hialurónico, sugiero esperar al menos 2 semanas y, a menudo, más tiempo; algunos profesionales prefieren 4 semanas. Para implantes o hilos permanentes, consulte con el profesional que le atiende sobre el momento más seguro.
Tatuajes y maquillaje permanente
La microaguja aplicada directamente sobre tatuajes o maquillaje permanente puede alterar el pigmento, provocar su migración y aumentar el riesgo de infección.
Generalmente les digo a las personas que eviten la microaguja directamente sobre los tatuajes, a menos que un especialista con experiencia esté planeando el procedimiento por un motivo específico.
Lo que recomiendo: tratar únicamente la piel no tatuada o consultar a un especialista con experiencia en el trabajo con zonas tatuadas.
Alergias conocidas a agentes anestésicos o ingredientes tópicos.
Si tiene una alergia documentada a los anestésicos tópicos o a los ingredientes comúnmente utilizados en los protocolos de cuidados posteriores (como ciertos antisépticos o antibióticos tópicos), lo consideraré una contraindicación hasta que encontremos alternativas.
Siempre pregunto sobre las alergias porque las reacciones durante o después del procedimiento pueden complicar la curación.
Lo que recomiendo: informar sobre todas las alergias y reacciones previas. A menudo podemos elegir productos alternativos, pero esto podría afectar la programación o la decisión de proceder.
Infecciones virales recientes o enfermedades sistémicas
Si actualmente está enfermo con una infección sistémica (por ejemplo, una enfermedad similar a la gripe o COVID-19), pospondría la microaguja hasta que se haya recuperado.
Hago hincapié primero en el descanso y la recuperación; el cuerpo se cura mejor cuando no está luchando contra otra enfermedad activa.
Lo que recomiendo: reprogramar después de una recuperación completa y asegurarse de que no haya fiebre activa ni síntomas sistémicos.
Tabla: Referencia rápida de contraindicaciones comunes
Considero que las tablas son útiles para tomar decisiones clínicas rápidamente. A continuación, se presenta un resumen conciso de las contraindicaciones comunes, su importancia y mis recomendaciones habituales.
| Condición/Situación | Por qué es una preocupación | Mi recomendación práctica |
|---|---|---|
| Infección cutánea activa (bacteriana/fúngica/herpética) | Riesgo de infección más profunda y propagación | Tratar la infección y esperar hasta que se resuelva |
| Acné inflamatorio activo, rosácea, psoriasis, eczema. | Puede empeorar la inflamación o desencadenar lesiones. | Controle primero la condición; reevalúe cuando esté estable |
| Historia de queloides/cicatrización hipertrófica | Riesgo de cicatrización anormal | Evite la microaguja en zonas propensas; considere alternativas |
| Isotretinoína sistémica (actual/reciente) | Cicatrización deficiente; riesgo de cicatrices | Evitar durante la terapia; esperar de 6 a 12 meses después de finalizarla |
| Terapia anticoagulante / trastornos hemorrágicos | Sangrado excesivo, hematomas, hematomas | Consulte al médico que prescribe; puede posponer o ajustar los medicamentos. |
| Inmunosupresión/quimioterapia | Cicatrización deficiente, riesgo de infección | Posponer hasta la recuperación inmunológica; obtener autorización |
| diabetes no controlada | Mala cicatrización, infección | Lograr el control glucémico; obtener autorización médica |
| Cáncer de piel activo o escisión reciente | Interfiere con la atención del cáncer | Espere hasta que el especialista lo autorice. |
| Tratamientos ablativos recientes (láser/peeling) | Trauma acumulativo, curación retardada | Siga el intervalo recomendado por el médico |
| Embarazo / lactancia | Datos de seguridad limitados; contraindicaciones tópicas | Posponer hasta después del embarazo/la lactancia |
| Rellenos, hilos e implantes recientes | Riesgo de infección, desplazamiento del relleno | Espere el intervalo recomendado; consulte al médico tratante |
| Tatuajes/maquillaje permanente | Alteración de la pigmentación, infección. | Evite el tratamiento directo; consulte a un especialista. |
| Alergias a agentes tópicos/anestésicos | Riesgo de reacción alérgica | Utilice alternativas o posponga |
Consideraciones especiales: melasma, hiperpigmentación y tipos de piel más oscuros.
Si tienes melasma o pieles más oscuras tipo Fitzpatrick, procedo con precaución. La microaguja puede ser útil para algunos problemas de pigmentación, pero también puede provocar hiperpigmentación postinflamatoria (HPI) si no se realiza correctamente.
Generalmente recomiendo un régimen pretratamiento cuidadoso (que incluye protección solar y agentes tópicos como hidroquinona o ácido tranexámico cuando corresponda) y un tratamiento conservador. En algunos casos, la microaguja combinada con crioterapia o peelings químicos está contraindicada para el melasma.
Recomiendo: consultar con un dermatólogo con experiencia en piel pigmentada, seguir un plan de pretratamiento para estabilizar el melasma y utilizar técnicas conservadoras. Si el melasma está activo o inestable, posponer el tratamiento.
Dispositivos de microagujas para uso doméstico: precaución adicional
Los dermarollers y microagujas para uso doméstico están ampliamente disponibles, pero conllevan riesgos diferentes a los de los tratamientos en consultorio. Me preocupa la esterilización inadecuada, compartir dispositivos, la longitud excesiva de las agujas y el uso agresivo que aumenta el riesgo de infección y cicatrices.
A menudo les digo a las personas que los procedimientos en el consultorio son más seguros debido a los dispositivos de grado médico, la técnica estéril y los proveedores capacitados.
Lo que recomiendo: si estás considerando usarlo en casa, usa dispositivos con agujas cortas (normalmente de 0,25 mm) y mantén una higiene estricta. Sin embargo, para tratamientos más profundos o si tienes alguna de las contraindicaciones mencionadas, consulta con un profesional en lugar de hacerlo tú mismo.
Interacciones medicamentosas y tópicas: qué pregunto antes del tratamiento
Antes de aceptar la microaguja para cualquier persona, reviso los medicamentos y productos tópicos que podrían afectar la seguridad:
- Isotretinoína sistémica (Accutane): evitar durante el uso y durante el período de espera recomendado después del mismo.
- Anticoagulantes y antiagregantes plaquetarios: evaluar riesgo de sangrado.
- Inmunosupresores sistémicos o biológicos: analizar el riesgo y el momento oportuno.
- Retinoides tópicos y exfoliantes: a menudo se suspenden antes y después del tratamiento para reducir la irritación.
- Antibióticos o antivirales orales: pueden usarse de manera profiláctica en casos selectos (por ejemplo, antecedentes de herpes labial).
Recomiendo la divulgación completa de los medicamentos y suplementos, incluidos los AINE de venta libre y los suplementos a base de hierbas que afectan el sangrado (como el aceite de pescado, el ginkgo o la vitamina E en dosis altas), para poder asesorar adecuadamente.
Cómo evalúo la candidatura durante una consulta
Cuando alguien me pregunta sobre la microaguja, adopto un enfoque estructurado:
- Historial médico: reviso enfermedades sistémicas, medicamentos, estado de embarazo y condiciones autoinmunes.
- Historial dermatológico: pregunto sobre antecedentes de herpes labial, acné, queloides, problemas de pigmentación y procedimientos previos.
- Examen de la piel: inspecciono el área de tratamiento para detectar lesiones activas, quemaduras solares o irritación.
- Expectativas: Discuto objetivos, riesgos, número de sesiones y resultados realistas.
- Plan: Asesoro sobre los pasos previos al tratamiento (suspender los retinoides tópicos, estabilizar la enfermedad) y los cuidados posteriores.
Animo al diálogo abierto porque el plan más seguro depende de los factores de riesgo individuales.
Alternativas cuando la microaguja no es adecuada
Si la microaguja está contraindicada, a menudo sugiero alternativas más seguras dependiendo del problema que quieras tratar.
- Peelings químicos superficiales o exfoliación química suave y ligera: para texturas suaves y pigmentación superficial, si corresponde.
- Microdermoabrasión: opción no invasiva para la textura de la piel; menor riesgo de infección.
- Terapias médicas tópicas: retinoides, hidroquinona, ácido tranexámico o cremas recetadas para la pigmentación y la textura a lo largo del tiempo.
- Opciones inyectables: en casos selectos, los rellenos o neuromoduladores pueden abordar la pérdida de volumen o las líneas sin rejuvenecimiento.
- Terapias con láser o luz: aunque algunos láseres comparten contraindicaciones similares, ciertos láseres no ablativos pueden considerarse cuando la microaguja no es apropiada; siempre evalúe caso por caso.
- Tratamientos específicos para cicatrices: queloides o cicatrices hipertróficas, inyecciones de esteroides, láminas de silicona u opciones quirúrgicas con planificación especializada.
Siempre adapto las alternativas a la condición y al perfil médico de la persona.
Consejos de seguridad y señales de alerta que utilizo en la práctica
Ofrezco a las personas consejos prácticos de seguridad para que puedan detectar señales de alerta y tomar decisiones informadas.
- Elija un profesional con experiencia y licencia. Prefiero profesionales con formación médica o entornos supervisados.
- Verificar los protocolos de esterilización de la clínica y que se utilicen agujas desechables de un solo uso para los tratamientos en el consultorio.
- Tenga cuidado con los precios agresivos o las ofertas que incentivan a omitir la revisión médica previa al procedimiento.
- Si nota dolor inusual, enrojecimiento que se extiende, fiebre o pus después del tratamiento, busque atención médica urgente.
- Evite la exposición al sol y el bronceado inmediatamente antes y después de la microaguja para reducir las complicaciones pigmentarias.
- Siga estrictamente las instrucciones de cuidado posterior para limpiadores, ungüentos y protectores solares, ya que estos influyen en la curación y los resultados.
Si siente algo “extraño” durante o después del procedimiento, recomiendo a las personas que se comuniquen con su proveedor lo antes posible.
Preguntas frecuentes que recibo de los pacientes
A menudo me hacen preguntas predecibles. Aquí están mis respuestas típicas:
- ¿Puedo someterme a microagujas si tengo cicatrices de acné? Sí, en muchos casos, la microaguja es eficaz para las cicatrices de acné atróficas, pero no durante el acné inflamatorio activo.
- Si soy propenso al herpes labial, ¿puedo someterme a microagujas? Es posible. Suelo recomendar profilaxis antiviral y asegurarme de que no haya lesiones activas.
- ¿Es segura la microaguja en todos los tonos de piel? La microaguja suele ser más segura que muchos láseres para pieles más oscuras, pero conlleva riesgo de hiperpigmentación postoperatoria (HPI); es importante usar una técnica cuidadosa y realizar los tratamientos antes y después.
- ¿Pueden los adolescentes someterse a microagujas? Soy cauteloso con la piel joven; si se trata de un adolescente, evalúo el problema subyacente y suelo preferir primero los tratamientos conservadores.
- ¿Cuántas sesiones se necesitan? Depende del problema; de 3 a 6 sesiones con semanas de diferencia es habitual para muchas indicaciones, pero siempre adapto el plan.
Consideraciones posteriores al procedimiento y cuándo contactar a un médico
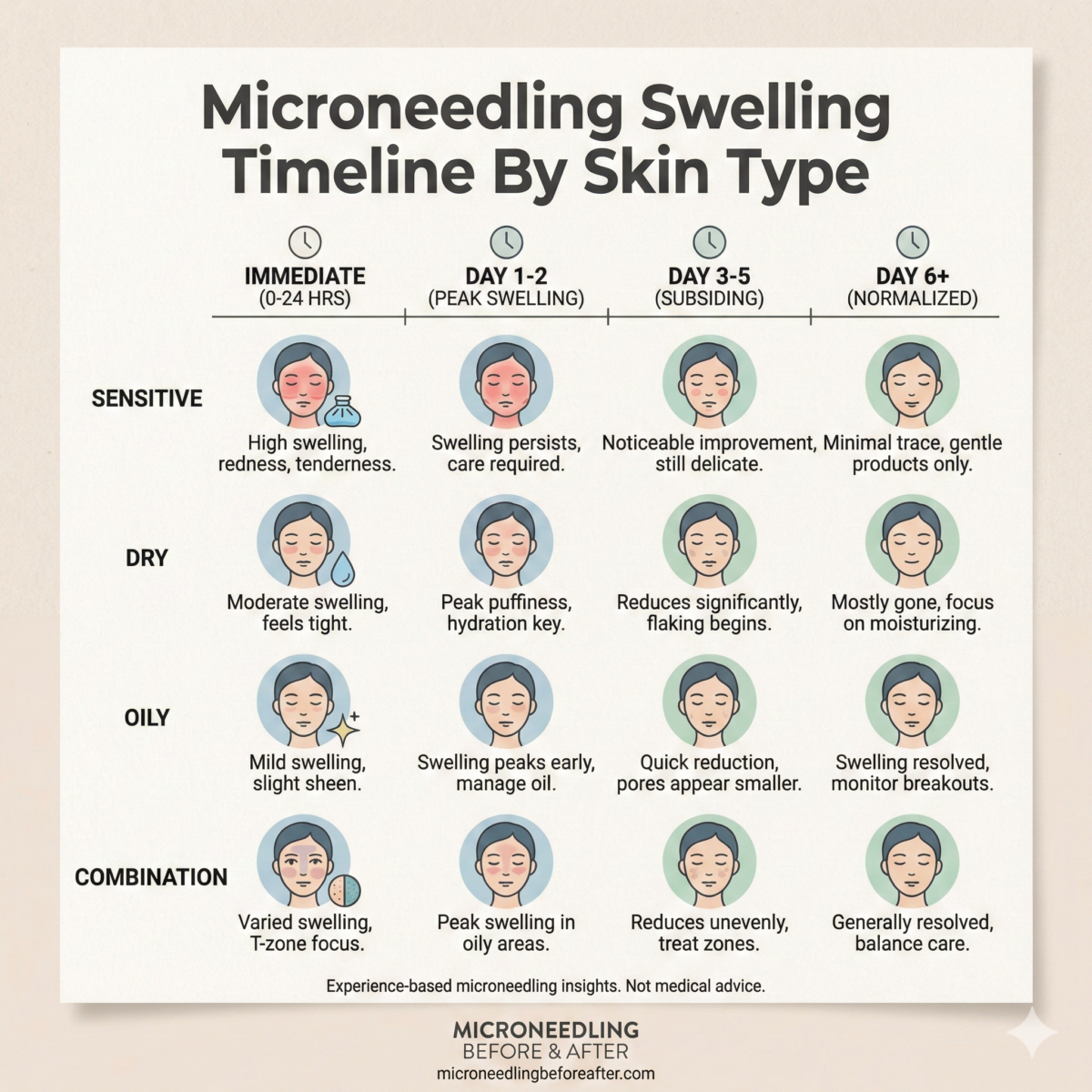
Tras la microaguja, las reacciones normales incluyen enrojecimiento, inflamación leve y sangrado o hematomas localizados que desaparecen en días. Use limpiadores suaves, cremas hidratantes y protectores solares según las indicaciones.
Comuníquese con su médico si experimenta un aumento del dolor, hinchazón que dura más de unos pocos días, enrojecimiento que se extiende, fiebre, pus o si nota signos de una reacción alérgica, como urticaria o dificultad para respirar.
Les digo a las personas que la atención rápida reduce el riesgo de que las complicaciones se agraven.
Lista de verificación final que utilizo antes de recomendar la microaguja
Cuando pienso si la microaguja es apropiada, mentalmente repaso esta lista de verificación:
- ¿Está la piel libre de infección activa o enfermedad inflamatoria en la zona?
- ¿Existen enfermedades sistémicas o medicamentos que afecten la curación?
- ¿El embarazo o la lactancia materna son un factor?
- ¿Existen antecedentes de cicatrices anormales o trastornos hemorrágicos?
- ¿Se han completado procedimientos o tratamientos recientes en un período de tiempo seguro?
- ¿Está el paciente informado sobre las alternativas, los riesgos y las expectativas realistas?
Si algún punto me genera preocupación, pospongo o adapto el plan, o bien recurro a un especialista.
Conclusión
La microaguja puede ser una herramienta eficaz para muchos problemas de la piel, pero no es una solución universal. Siempre evalúo a la persona en su totalidad: historial médico, medicación actual, estado de la piel y expectativas, antes de recomendar la microaguja. Hay situaciones en las que claramente no la realizaría o en las que requeriría precauciones específicas: infecciones activas, afecciones sistémicas no controladas, uso reciente de isotretinoína, inmunosupresión, embarazo y antecedentes de queloides, entre otras.
Si está considerando la microaguja, le recomiendo tener una conversación sincera con un profesional cualificado, informar sobre su historial médico completo y seguir estrictamente las instrucciones de cuidado antes y después del tratamiento. Si bien se evita la microaguja por razones de seguridad, generalmente existen alternativas más seguras que pueden ayudarle a alcanzar sus objetivos sin poner en riesgo su salud.
Si lo desea, puedo ayudarle a analizar un historial médico o una inquietud específica para determinar si la microaguja podría ser apropiada para usted y qué momento o alternativas sugeriría.