? What specific microneedling protocol will best achieve the treatment outcome I intend for a particular patient?
Microneedling Protocol Differences By Treatment Goal
I will present a structured, detailed review of how microneedling protocols change according to treatment objective. I aim to give practical, evidence-informed guidance so I can select depths, devices, adjuncts, and aftercare that optimize safety and efficacy for each indication.
Overview of microneedling and clinical endpoints
I consider microneedling an umbrella term describing controlled micro-injury to the skin to induce remodeling and permit transdermal delivery. I will highlight that treatment parameters — needle length, device type, number of passes, endpoint, and adjuncts — are the levers I adjust to meet specific goals.
Biological rationale and expected responses
I understand that microneedling stimulates wound healing cascades, collagen and elastin production, and can modulate pigmentation and scarring. I will note that outcomes depend on intensity of injury, focal anatomy, and patient biology including age, hormonal status, and skin type.
Device types and practical differences
I will summarize the main device categories and how they influence protocol selection. Device choice affects precision, depth control, patient comfort, and compatibility with adjuncts such as radiofrequency or topical biologics.
Manual rollers, automated pens, and RF microneedling
I prefer automated pens for facial work because they provide consistent vertical needle entry and adjustable depth settings. I will use RF microneedling when I need thermal coagulation in addition to mechanical injury for skin tightening or scar remodeling.
Needle configuration, cartridge selection, and sterility concerns
I select cartridges based on needle length and gauge; I always use single-patient sterile tips to minimize infection risk. I will emphasize that needle gauge changes tissue trauma and bleeding risk — thinner needles cause less bleeding, while thicker needles may create a larger channel for topical delivery.
Key treatment variables and clinical endpoints
I will define the parameters I adjust and the clinical endpoints I seek during treatment. Being explicit about these variables helps standardize protocols and manage expectations.
Needle depth, number of passes, speed, and endpoint
I typically vary needle depth from 0.25 mm for superficial rejuvenation up to 3.5 mm for deep acne scars or body stretch marks. I assess endpoint by tissue response: visible pinpoint bleeding and serous oozing indicate adequate dermal disruption for remodeling in many scar protocols, while erythema without bleeding may be sufficient for superficial rejuvenation.
Frequency and course of treatments
I usually space treatments according to depth: shallow treatments every 2–4 weeks and deeper or aggressive protocols every 6–8 weeks to allow remodeling. I will tailor total number of sessions to the indication — for example, 3–6 sessions for general rejuvenation and 4–8 (or more) for severe acne scarring.
Patient selection and Fitzpatrick skin types
I carefully evaluate patient history, medications, active skin disease, and Fitzpatrick skin type to determine risk of postinflammatory hyperpigmentation (PIH) and other complications. I will classify my approach differently for Fitzpatrick I–III versus IV–VI to reduce pigmentary sequelae.
Pre-treatment priming and risk mitigation
I often use a preconditioning regimen for higher-risk patients: topical retinoid or growth factor priming in lower-risk patients and cautious bleaching/tyrosinase inhibitors for darker skin types. I will stop retinoids when clinically necessary and recommend antiviral prophylaxis for patients with a history of herpes simplex when treating perioral areas.
Protocols by treatment goal — summary table
I will provide a high-level table to compare recommended parameters by goal. This will help me and readers quickly match objectives with typical device settings, endpoints, frequency, and adjuncts.
| Treatment Goal |
Typical Needle Depth (mm) |
Device Type |
Endpoint |
Frequency |
Common Adjuncts |
| Superficial skin rejuvenation (fine lines, texture) |
0.25–0.75 |
Automated pen |
Diffuse erythema, no to minimal bleeding |
Every 2–4 weeks, 3–6 sessions |
Topical growth factors, vitamin C |
| Acne scarring (rolling/boxcar) |
1.5–3.0 |
Automated pen or RF microneedling |
Pinpoint bleeding, gelatinous dermal exudate |
Every 6–8 weeks, 4–8+ sessions |
PRP/PRF, cross-fragmentation, subcision combo |
| Surgical or hypertrophic scars |
1.5–3.0 (deeper for tethered scars) |
Automated pen / RF microneedling |
Pinpoint bleeding, release of tethering |
Every 6–8 weeks |
Steroid injection adjunct, silicone sheeting |
| Hyperpigmentation / melasma |
0.25–1.0 (cautious) |
Automated pen |
Mild erythema, avoid heavy bleeding |
Every 3–6 weeks, conservative approach |
Topical tranexamic acid, hydroquinone alternatives |
| Hair restoration (scalp) |
0.5–2.5 |
Automated pen |
Mild bleeding acceptable |
Every 2–6 weeks depending on depth |
PRP/PRF, topical minoxidil |
| Stretch marks (striae) |
1.5–3.5 |
Automated pen or roller |
Pinpoint bleeding |
Every 6–8 weeks |
PRP, topical retinoids |
| Transdermal delivery (drug/peptide delivery) |
0.25–1.5 |
Automated pen |
No bleeding required for delivery-only protocols |
As needed |
Mesotherapy, peptides, corticosteroid delivery |
Superficial skin rejuvenation protocols
I perform superficial microneedling when the primary goals are improving skin tone, pore size, mild texture irregularities, and fine lines. I will generally use short needle lengths and fewer passes to minimize downtime and pigmentary risk.
Device settings and adjuncts for rejuvenation
I typically set needle depth between 0.25 and 0.75 mm for facial rejuvenation. I will apply topical growth factors, peptides, or vitamin C either immediately after treatment or via mesotherapy to leverage increased permeability.
Frequency, expected results, and downtime
I schedule sessions every 2–4 weeks and expect gradual textural improvements after 3–6 treatments. I advise patients of 24–72 hours of erythema and superficial flaking, but minimal social downtime for most.
Acne scarring protocols
I approach acne scarring with a protocol that balances depth for collagen induction against potential for PIH, especially in darker skin types. I select deeper settings and allow longer healing intervals.
Needle depth, passes, and combination strategies
For rolling and boxcar scars I commonly use 1.5–3.0 mm, with multiple passes targeted to the scarred regions. I often combine microneedling with PRP/PRF or fractional RF to enhance collagen remodeling and sometimes pair with subcision to release deep tethered areas.
Timeline, outcomes, and managing expectations
I space sessions every 6–8 weeks and plan for 4–8+ sessions depending on scar severity. I counsel that significant improvement often requires adjunctive therapies and that full maturation may take several months.
Surgical and hypertrophic scar protocols
I treat surgical scars with deeper microneedling to soften texture, increase pliability, and permit steroid or enzymatic adjuncts. I tailor my approach based on scar age and vascularity.
Strategies for hypertrophic and keloid-prone patients
I exercise caution in keloid-prone patients and typically avoid aggressive protocols; instead I use conservative microneedling combined with intralesional steroid delivery. I will monitor for signs of hypertrophic scarring and consider referral when lesions are active.
Device choice and depth considerations
For older, flat scars I may use 1.5–2.5 mm; for tethered scars combined subcision with microneedling at similar depths may produce better contour improvement. I will use RF microneedling in some cases to introduce thermal remodeling but take care to not exacerbate scar hypertrophy.
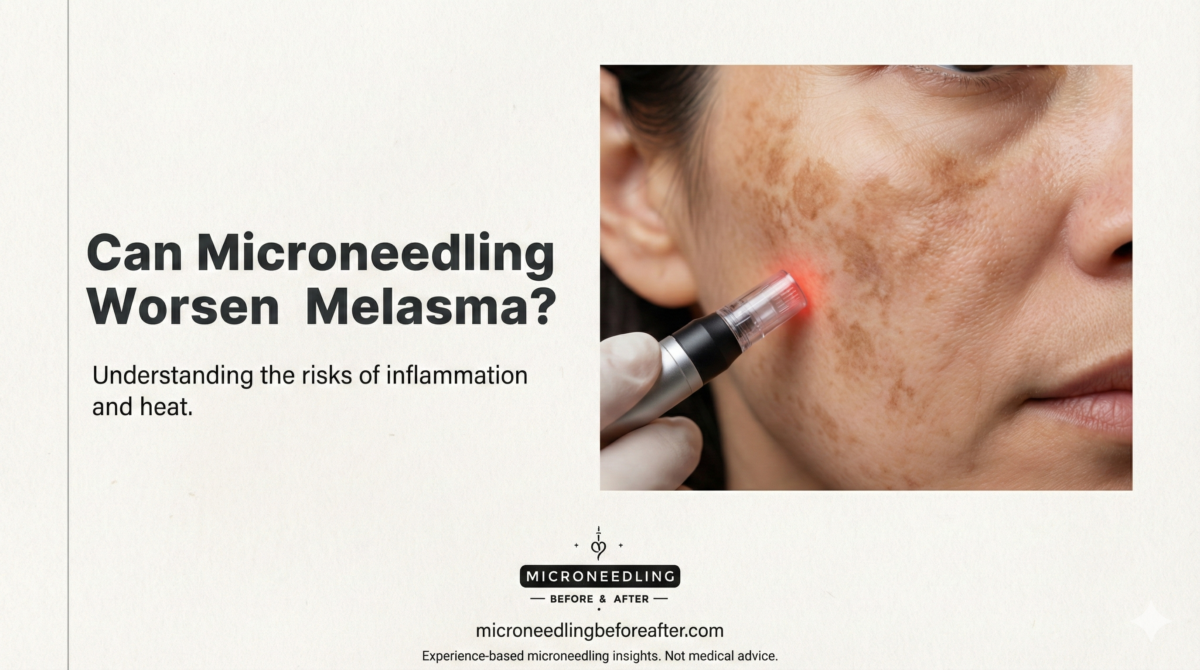
Hyperpigmentation and melasma protocols
I approach pigmentary disorders cautiously because microneedling can both help and harm pigment. I reduce depth and frequency while using adjunctive topical agents to prevent PIH.
Conservative protocols and adjunctive topical therapy
I often select 0.25–1.0 mm depth with minimal bleeding and use tranexamic acid, vitamin C, or azelaic acid in conjunction. I will avoid aggressive treatment in active melasma and prioritize priming with topical agents for several weeks prior.
Risk reduction for PIH
I institute strict sun protection and may start topical hydroquinone or non-hydroquinone alternatives before treatment for higher-risk skin types. I will avoid repeat sessions until inflammation resolves and appear cautious with any protocol that produces heavy inflammation.
Hair restoration protocols
I use microneedling in androgenetic alopecia and other hair loss conditions to enhance transdermal delivery of growth factors and stimulate follicles. Depth selection is scalp-specific and often deeper than facial settings.
Depth, PRP/PRF adjuncts, and treatment cadence
I use 0.5–2.5 mm depending on scalp area and hair density; typical practice uses 1.5 mm for vertex areas. I commonly pair microneedling with PRP/PRF and schedule sessions every 4–6 weeks for 3–6 treatments before reassessment.
Outcome expectations and combination therapy
I inform patients that results are incremental and often better when combined with topical or oral therapies like topical minoxidil or antiandrogens. I monitor for scalp infections and folliculitis and emphasize adherence to a regular maintenance program.
Stretch mark (striae) protocols
I treat striae with relatively aggressive depth to reach lower dermis because these lesions involve deeper dermal disruption. I manage patient expectations about partial rather than complete resolution.
Needle depth and adjunctive therapies
I commonly use 1.5–3.5 mm depths on body areas with thicker dermis and combine with PRP or topical retinoids to stimulate remodeling. I will space treatments every 6–8 weeks and recommend several sessions for meaningful texture changes.
Safety considerations for bodywork
I perform test areas when treating large regions and counsel on pain management during longer sessions. I will consider local anesthesia for larger or deeper sessions to improve patient comfort.
Transdermal drug and biologic delivery
I employ microneedling to enhance penetration of topicals, peptides, small molecules, or biologic products with minimal systemic absorption. Depth and timing relative to topical application are key variables.
Depth and timing for optimal delivery
For most topical delivery purposes I use 0.25–1.5 mm to produce channels without heavy scabbing. I apply the therapeutic agent immediately post-procedure to leverage open microchannels and often occlude briefly to increase uptake.
Safety and pharmacokinetic considerations
I ensure the applied agents are appropriate for transdermal use and counsel patients regarding potential systemic exposure. I avoid unapproved or unvalidated compounds and adhere to local regulatory guidance.
Periorbital and lip area protocols
I treat periorbital skin and lips conservatively because of thin dermis and higher risk of bruising and pigment changes. I adjust depth and technique to preserve safety.
Depth adjustments and technique nuances
I typically use 0.25–0.5 mm around the eyelids and 0.5–1.0 mm for perioral areas. I perform minimal passes, maintain gentle pressure, and avoid aggressive endpoints in these delicate zones.
Adjuncts and anesthesia
I prefer topical anesthetic creams and careful patient positioning for comfort. I combine with PRP or hyaluronic acid fillers only when clinically indicated and with experience in these areas.
Anaesthesia, pain control, and patient comfort
I balance adequate analgesia with safety, especially for deeper or longer treatments. I provide topical anesthesia for most facial treatments and consider nerve blocks for extensive body sessions.
Topical anesthetics, numbing duration, and safety
I apply topical anesthetics 30–45 minutes prior and use occlusion to improve penetration when needed. I am cautious with epinephrine-containing mixtures on the face and avoid repeated full-face nerve blocks unless trained and indicated.
Infection control, contraindications, and safety checklist
I adhere to strict aseptic technique, screening protocols, and contraindication review to minimize complications. I document informed consent and baseline photography as part of standard practice.
Absolute and relative contraindications
I will not treat active infection, severe isotretinoin use within prior 6–12 months, active autoimmune disease with instability, or unhealed wounds. I use caution with pregnancy, anticoagulation, keloid predisposition, and uncontrolled diabetes.
Complication recognition and management
I monitor for infection, prolonged erythema, scarring, and PIH. I treat bacterial infection promptly with antibiotics and initiate early management for PIH with topical lighteners and sun protection.
Post-treatment care and expectations
I provide explicit, written post-care instructions to control inflammation, prevent infection, and enhance results. Patient adherence heavily influences outcomes, so I review do’s and don’ts verbally and in print.
Immediate post-care and first week
I recommend gentle cleansing, avoidance of makeup for 24 hours when possible, continuous sunscreen use, and cryotherapy for swelling. I advise against active ingredients like retinoids and certain acids for at least 48–72 hours or longer if the epidermis is disrupted.
Long-term skin care and maintenance schedule
I encourage a maintenance program tailored to the original indication — for example, quarterly superficial treatments for ongoing rejuvenation or periodic PRP boosters for hair maintenance. I will also emphasize consistent sun protection and topical agents that complement microneedling gains.
Combining microneedling with other modalities
I use combination therapy when synergistic benefits outweigh added cost or downtime. I will time combinations carefully — either in the same session (e.g., microneedling + PRP) or staged across weeks (e.g., microneedling preceding a laser).
PRP/PRF, chemical peels, lasers, and fillers
I often combine microneedling with PRP/PRF to amplify collagenogenic stimulus, particularly for scarring and rejuvenation. I avoid aggressive ablative lasers immediately after microneedling; if combining, I schedule lasers after initial microneedling healing or vice versa based on risks.
Documentation, consent, and outcome measurement
I document baseline photos, device settings, needle depth, number of passes, adjuncts used, and patient-reported pain scores. I also set measurable outcome goals and timelines for follow-up assessment.
Standardized photography and outcome scales
I use standardized photography and scar grading scales (e.g., global acne scarring classification) to quantify progress. I will also solicit patient-reported outcome measures to capture subjective satisfaction.
Troubleshooting common problems
I address suboptimal response, PIH, persistent erythema, and infection with targeted interventions and protocol modifications. I rarely abandon microneedling but will modify strategy and consider alternative modalities when appropriate.
Nonresponse and protocol escalation
If a patient does not respond after an adequate trial, I escalate by increasing depth, adding adjuncts like PRP, or combining with subcision/RF. I will reassess skin type, compliance, and underlying pathology before changing course.
Managing PIH and extended inflammation
I initiate conservative lightening regimens and avoid further inflammatory triggers when PIH occurs. I consider topical tranexamic acid, azelaic acid, and short courses of low-potency steroids in inflammatory flares with specialist input.
Practical tables for clinic use
I provide a clinical cheat sheet summarizing indications, depths, frequencies, and adjuncts for routine reference in practice.
| Indication |
Depth (mm) |
Frequency |
Endpoint |
Common Adjunct |
| Fine lines / superficial texture |
0.25–0.75 |
2–4 wks |
Erythema |
Topical peptides |
| Moderate acne scarring |
1.5–2.5 |
6–8 wks |
Pinpoint bleeding |
PRP/PRF |
| Severe acne scarring |
2.5–3.5 |
6–10 wks |
Bleeding + remodeling |
RF, subcision |
| Melasma / hyperpigmentation |
0.25–1.0 (conservative) |
3–6 wks |
Mild erythema |
Tranexamic acid |
| Scalp hair restoration |
1.0–2.5 |
4–6 wks |
Mild bleeding acceptable |
PRP, topical minoxidil |
| Striae |
1.5–3.5 |
6–8 wks |
Bleeding |
PRP, topical retinoids |
| Pre/Post Care Checklist |
| Review medications and contraindications |
| Pre-treat with topical agents if indicated |
| Ensure sterile, single-use needles and cartridges |
| Apply topical anesthetic as needed |
| Post-treatment: gentle cleansing, no makeup 24 h, sunscreen, avoid retinoids for 48–72 h |
| Provide emergency contact for infection or adverse events |
Ethical and regulatory considerations
I ensure that all products used with microneedling are within regulatory frameworks and that off-label uses are disclosed in consent. I will stay current with local regulations related to autologous blood products (e.g., PRP/PRF) and device approvals.
Informed consent and patient education
I obtain written informed consent that outlines expected benefits, risks, alternative options, and costs. I make sure patients understand downtime, need for multiple treatments, and maintenance requirements.
Final thoughts and clinical decision-making framework
I approach microneedling as a customizable tool, not a one-size-fits-all treatment. By systematically matching needle depth, device, endpoint, adjuncts, and aftercare to the specific treatment goal and patient phenotype, I can optimize outcomes and minimize complications.
Practical algorithm I use in clinic
- Define primary treatment goal and set realistic outcome expectations.
- Assess skin type, scar type, and medical history.
- Choose device, depth, and endpoint appropriate for the goal.
- Select adjuncts such as PRP, topical agents, or combination therapies.
- Provide pre-treatment priming and detailed post-care instructions.
- Document settings and outcomes, and adapt the plan based on response.
I will use this framework to select microneedling protocols reliably and reproducibly. Applying these structured choices will help ensure I offer each patient a protocol that is both safe and tailored to their goals.