How long will my face remain swollen after microneedling, and how does my skin type influence that timeline?
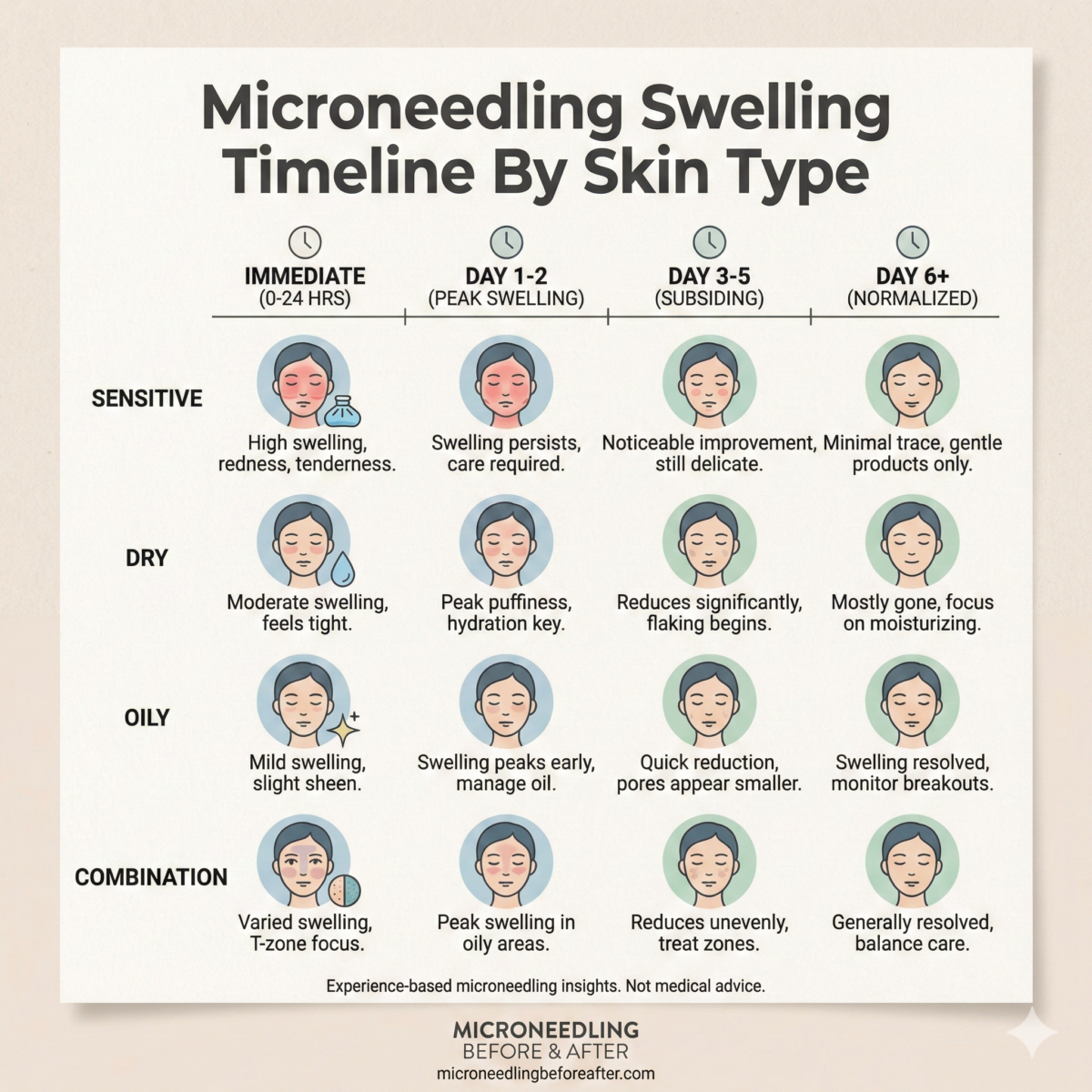
Microneedling Swelling Timeline By Skin Type
I will explain how microneedling typically causes swelling, why the response varies across skin types, and what realistic timelines look like. I will also provide practical management strategies so you can plan treatments and expectations appropriately.
Why swelling occurs after microneedling
I recognize that microneedling purposefully creates controlled micro-injuries in the skin to stimulate collagen and elastin production. Swelling is a normal inflammatory response as fluid and immune cells rush to the treated areas to begin repair, and the degree of swelling depends on several physiologic and treatment variables.
How I classify skin types for swelling expectations
I use common dermatologic and cosmetic categories: normal, dry, oily, combination, sensitive, acne-prone, rosacea-prone, darker (higher Fitzpatrick) skin tones, fair/thin/aging skin, and those with inflammatory skin conditions like eczema or psoriasis. I find this classification practical for anticipating swelling patterns and advising aftercare.
General factors that influence swelling
I will outline the main variables that change how much and how long swelling will last so you can understand why two people may experience different timelines after the same procedure.
- Treatment depth and device: Professional devices with needles at 1.5 mm or deeper and radiofrequency-microneedling cause more swelling than shallow at-home devices.
- Number of passes and treatment intensity: More passes and firmer pressure increase swelling.
- Anatomic area treated: Periorbital, lip, and forehead regions often swell more due to thinner skin and loose subcutaneous tissues.
- Pre-existing inflammation and skin conditions: Rosacea and acne can amplify swelling.
- Systemic factors: Medications (blood thinners), recent alcohol, salt intake, sleep, and hydration influence fluid retention.
- Technique and topical anesthesia: Use of topical anesthetics, whether vasoconstrictors were used, and post-treatment cooling alter swelling onset and duration.
Typical swelling timeline stages
I find it useful to conceptually divide the healing into stages so patients can track progress and know what to expect at each interval.
| Stage | Timeframe | Typical signs |
|---|---|---|
| Immediate | 0–6 hours | Erythema, pinpoint bleeding, initial puffiness |
| Acute | 6–72 hours | Peak swelling typically within 24–48 hours, warmth, tenderness |
| Early recovery | 3–7 days | Redness decreases, swelling subsides substantially, skin tightness |
| Late recovery | 1–4 weeks | Residual erythema resolves, collagen remodeling begins |
| Full recovery | 4–12 weeks | Visual improvements mature, minimal swelling or none |
I include this table to make the overall pattern easier to understand and to give a frame of reference for more specific skin-type timelines.
Swelling timeline by skin type — summary table
I provide a compact comparison so you can quickly scan expectations for your skin type. These are general estimates; individual responses vary.
| Skin Type | Typical Peak Swelling | Usual Duration of Noticeable Swelling | Notes |
|---|---|---|---|
| Normal | 24–48 hours | 2–5 days | Predictable response; rapid recovery in most cases |
| Dry | 24–48 hours | 3–7 days | May feel tight and slightly longer to exfoliate |
| Oily | 24–72 hours | 2–6 days | Outlet for sebum is unaffected; inflammation may take slightly variable course |
| Combination | 24–48 hours | 2–6 days | T-zone regions may recover differently from cheeks |
| Sensitive | 12–72 hours | 4–10 days | Heightened inflammatory response; redness and swelling can be prolonged |
| Acne-prone | 24–72 hours | 3–10 days | Active acne may flare; infections are a risk if contraindications ignored |
| Rosacea-prone | 12–72 hours | 5–14 days | Marked flushing and swelling possible; proceed cautiously |
| Fitzpatrick IV–VI (darker skin) | 24–72 hours | 3–10 days | Swelling similar or slightly prolonged; risk of PIH requires cautious aftercare |
| Fair/thin/aging skin | 12–48 hours | 2–5 days | Thinner skin may bruise or swell more readily |
| Eczema/Psoriasis | 12–72 hours | 5–14 days or longer | Flare risk; must be managed with dermatologist input |
I encourage using the table as a starting point rather than a definitive timeline for every individual case.
Normal skin
I consider “normal” skin to have a balanced sebum production and no chronic inflammatory conditions. I typically tell patients with this skin type to expect predictable inflammatory responses.
- Peak swelling: 24–48 hours
- Noticeable swelling: 2–5 days
- Management tips: Gentle cooling and a basic barrier-restoring moisturizer help the skin recover quickly. I advise avoiding harsh actives for the first 72 hours.
Dry skin
I recognize that dry skin often has a compromised barrier and reduced natural oils, which can make it feel tighter and more sensitive after treatment.
- Peak swelling: 24–48 hours
- Noticeable swelling: 3–7 days
- Key considerations: I recommend using occlusive emollients and humectants (e.g., hyaluronic acid followed by a barrier cream) to reduce tightness and promote comfort. Avoid alcohol-based toners or astringents post-treatment.
Oily skin
I find that oily skin produces a relatively similar swelling response but may handle irritation differently due to thicker sebaceous activity.
- Peak swelling: 24–72 hours
- Noticeable swelling: 2–6 days
- Key considerations: I recommend light, non-comedogenic hydrating products and avoid heavy oil-based creams that can trap heat or bacteria. Monitor for acneiform reactions if active acne is present.
Combination skin
I explain that combination skin may experience mixed timelines because different facial zones heal at different rates.
- Peak swelling: 24–48 hours
- Noticeable swelling: 2–6 days
- Key considerations: I suggest zone-based aftercare: richer emollients on cheeks if dry, lighter gels on the T-zone if oily. This balances hydration without increasing irritation.
Sensitive skin
I note that sensitive skin can have amplified inflammatory responses to injury and topical agents, which makes swelling and redness potentially more pronounced and prolonged.
- Peak swelling: 12–72 hours
- Noticeable swelling: 4–10 days
- Key considerations: I advise patch testing, using minimal passes during treatment, and employing anti-inflammatory soothing agents like topical niacinamide or centella asiatica after professional approval. I often recommend consulting a dermatologist to tailor settings.
Acne-prone skin
I discuss that acne-prone skin presents a special challenge because microneedling can transiently spread bacteria if performed over active pustules and may exacerbate inflammation if not properly selected.
- Peak swelling: 24–72 hours
- Noticeable swelling: 3–10 days
- Key considerations: I generally avoid treating active inflamed acne with microneedling. If treating acne-scarring rather than active lesions, strict antiseptic technique and appropriate topical antimicrobials may be used. I monitor for signs of infection.
Rosacea-prone skin
I emphasize caution for rosacea because capillary fragility and neurovascular hyperreactivity can result in extended flushing and swelling.
- Peak swelling: 12–72 hours
- Noticeable swelling: 5–14 days
- Key considerations: I recommend conservative needle depths, pre- and post-treatment anti-inflammatory regimens (per dermatologist guidance), and consideration of alternative modalities if rosacea is active. I advise clear informed consent about the risk of extended erythema.
Fitzpatrick IV–VI (darker skin tones)
I explain that darker skin tones do not necessarily experience more swelling, but there is a heightened concern for post-inflammatory hyperpigmentation (PIH) if inflammation is prolonged.
- Peak swelling: 24–72 hours
- Noticeable swelling: 3–10 days
- Key considerations: I suggest pre-treatment optimization (retinoid tapering, skin-lightening cosmeceuticals if indicated) and cautious post-treatment management to limit inflammation and potential PIH. I recommend sunscreen and avoidance of heat/inflammation.
Fair, thin, or aging skin
I note that thinner or aged skin may bruise or show edema more visibly, and the response can be quicker to occur because the dermis is less robust.
- Peak swelling: 12–48 hours
- Noticeable swelling: 2–5 days
- Key considerations: I favor lighter settings and a conservative approach. I instruct using gentle moisturizers and short, targeted treatments to prevent prolonged downtime.
Eczema or psoriasis
I stress that inflammatory skin disorders such as eczema or psoriasis require individualized planning because microneedling can potentially trigger flares.
- Peak swelling: 12–72 hours
- Noticeable swelling: 5–14 days or longer
- Key considerations: I typically coordinate with a treating dermatologist. If disease is controlled, limited superficial microneedling may be considered; if active, I recommend postponing. I advise close post-procedure monitoring for flare-ups.
Deep professional vs at-home microneedling — swelling differences
I compare professional in-office treatments with at-home devices to clarify expectations.
- Professional (0.75–3.0 mm and RF-microneedling): I explain these produce greater and longer swelling, often peaking at 24–48 hours and resolving over several days to two weeks depending on depth.
- Medical-grade RF-microneedling: I note this induces thermal injury in addition to microchannels, which can extend swelling and erythema beyond what needle-only devices cause.
- At-home dermarollers (0.2–0.5 mm): I state these cause minimal swelling, generally resolving within 24 hours or less, and primarily stimulate superficial exfoliation rather than significant collagen remodeling.
Immediate post-treatment care (0–24 hours)
I provide a stepwise list of actions that I recommend for the first day to minimize swelling and discomfort.
- Cooling: Apply clean cool compresses for short intervals (10–15 minutes on, 10–15 minutes off). Avoid prolonged cold that can cause vasoconstriction issues.
- Cleansing: Use a gentle, non-irritating cleanser to remove blood or lymphatic fluid.
- Topicals: I advise avoiding active topicals (retinoids, acids, potent vitamin C) and opting for bland, sterile hydrating serums or medical-grade hyaluronic acid if recommended.
- Positioning: Sleep with your head elevated the first night to reduce facial edema.
- Avoid: I caution against alcohol, NSAIDs (I ask patients to consult their provider if they are on prescribed anticoagulants), strenuous exercise, heat exposure, and hot showers for 24–48 hours.
First 48–72 hours — peak management
I outline what to expect and how to manage the typical peak swelling window.
- Expectation: I tell patients that swelling most often peaks within 24–48 hours but can remain elevated into day three for some skin types or deeper treatments.
- Anti-inflammatories: I sometimes recommend oral antihistamines or short courses of NSAIDs for discomfort if appropriate and approved by the provider. I avoid routine steroid use unless prescribed.
- Hydration and barrier repair: I encourage continued use of gentle moisturizers, occlusive creams at night, and avoidance of potential irritants.
- Sun protection: I stress strict UV avoidance and use of physical sunscreens when outdoors.
Days 3–7 — early recovery
I describe the trajectory of swelling and how to modify care as the inflammation subsides.
- Clinical course: I expect significant reduction in swelling by day 3–5 for most skin types, with residual redness and slight edema possible up to a week.
- Exfoliation: I advise against mechanical exfoliation and strong chemical peels until the skin barrier is fully restored.
- Makeup: I typically allow mineral or specially formulated cover cosmetics after 48–72 hours if there is no open bleeding or crusting, but I recommend patch testing.
Weeks 2–4 and beyond — remodeling phase
I explain the longer-term healing process where swelling has resolved but tissue remodeling continues.
- Clinical course: By 2–4 weeks most patients show minimal swelling; improvements in texture/pore size continue to emerge over 8–12 weeks as collagen remodels.
- Return to routine: I allow resumption of retinoids and active skincare per a staged plan after 1–3 weeks depending on skin’s recovery.
- Follow-up treatments: I discuss spacing treatments (commonly 4–6 weeks for collagen induction) and consider conservative approaches for sensitive or reactive skin types.
Practical table: Do’s and don’ts by timeframe
I include this table to provide concise guidance for common post-procedure questions.
| Timeframe | Do | Don’t |
|---|---|---|
| 0–24 hours | Cool intermittently, cleanse gently, use sterile hydrating products | Exercise, sauna, hot showers |
| 24–72 hours | Continue hydration, elevate head while sleeping, protect from sun | Apply active acids, retinoids, heavy makeup on open areas |
| 3–7 days | Gradually reintroduce gentle skincare, monitor for infection | Aggressive exfoliation or facial waxing |
| 1–4 weeks | Reintroduce most actives gradually if tolerated | Skip sunscreen or ignore prolonged redness |
I use this concise reference to reduce confusion and support safer recovery.
When to seek medical attention
I want to be clear about warning signs that require prompt evaluation.
- Excessive swelling beyond expected timeline: If swelling continues to worsen after 72 hours or becomes asymmetric and painful.
- Signs of infection: Increasing pain, warmth, spreading erythema, purulent drainage, or fever.
- Allergic reactions: Rapid, severe swelling, hives, difficulty breathing — seek emergency care.
- Prolonged, worsening hyperpigmentation or keloid formation concerns: Seek dermatologic follow-up.
I recommend contacting the treating clinician for any unexpected course.
Preventive strategies and pre-treatment optimization
I advise several steps to reduce the risk of severe swelling and complications before microneedling.
- Medical history review: I request disclosure of isotretinoin use, anticoagulants, active infections, and inflammatory conditions.
- Medication timing: I typically ask patients to avoid NSAIDs and high-dose vitamin E pre-procedure only as instructed, and to confirm isotretinoin cessation per dermatologic guidance.
- Skin preparation: I recommend pre-treating active inflammatory conditions and optimizing barrier function with hydration and, in some cases, topical anti-inflammatories.
- Conservative settings: For sensitive or high-risk skin types, I favor shallower needle depths and fewer passes.
I find that thoughtful pre-procedure planning reduces downtime and adverse outcomes.
Products and ingredients I recommend or avoid after microneedling
I give practical product guidance that I use when advising patients.
- Recommend immediately: Sterile saline, gentle hyaluronic acid serums, petroleum-based or ceramide-rich barrier creams, and physical sunscreens once healed.
- Use with caution: Niacinamide and centella asiatica can be soothing but should be introduced conservatively.
- Avoid for first 48–72 hours: Retinoids, alpha/beta hydroxy acids, ascorbic acid in high concentration, benzoyl peroxide, and alcohol-based toners.
- Antimicrobials: I consider topical antiseptics if indicated, but routine antibiotic creams are not always recommended unless there is a clear infection risk.
I emphasize individualized recommendations based on treatment intensity and skin type.
Managing swelling for specific concerns
I offer tailored strategies for some of the more challenging skin types.
- Rosacea-prone: I recommend pre-treatment control measures (topical or oral therapies) and post-treatment anti-inflammatories per dermatologic direction.
- Darker skin tones: I stress aggressive sun protection and consider topical lightening agents only after adequate healing to minimize PIH.
- Acne-prone: I avoid treating over active lesions and ensure antiseptic technique if scars are the target.
I adapt my approach to reduce complications and optimize outcomes for these groups.
Practical lifestyle considerations
I suggest practical behavioral adjustments that help minimize swelling and promote efficient healing.
- Sleep: I encourage sleeping elevated the first 1–3 nights.
- Diet: I recommend reducing salt and alcohol intake immediately before and after the treatment to limit edema.
- Activity: I advise avoiding high-intensity workouts, hot yoga, and heavy sweating for at least 48–72 hours.
- Travel: If you travel by air immediately after treatment, I advise extra cooling and hydration due to cabin pressure and dehydration effects.
I include these recommendations because modest lifestyle changes can materially affect recovery.
Repeat treatments and cumulative swelling
I explain how swelling may change with subsequent sessions.
- Cumulative effect: I note that repeated treatments spaced properly may produce less acute swelling as the skin adapts, but deeper or more aggressive sessions can reset the inflammatory response.
- Spacing: I generally recommend waiting 4–6 weeks between collagen induction sessions for facial treatments so swelling has fully resolved and remodeling is underway.
- Record-keeping: I advise tracking reactions after each session so settings can be modified if swelling was excessive in prior treatments.
I stress cautious progression to optimize long-term results without unnecessary downtime.
Checklist for post-microneedling care
I provide a short checklist I often give patients to simplify compliance.
- Cool with clean compresses for short intervals.
- Keep treated area clean; use gentle cleanser.
- Apply sterile hydrating serum and barrier cream at night.
- Avoid active ingredients for at least 72 hours.
- Use head elevation for sleep first night.
- Avoid strenuous exercise and heat sources for 48–72 hours.
- Protect from sun and apply SPF after epidermal healing.
- Contact provider for signs of infection or unexpected worsening.
I use this checklist to reduce confusion and increase safety.
Clinical scenarios and examples
I offer a few illustrative examples to help you contextualize timelines.
- Example 1 — 35-year-old with normal skin receiving 1.5 mm in-office microneedling: I would expect peak swelling at 24–48 hours with substantial improvement by day 4 and near-normal appearance by day 7.
- Example 2 — 45-year-old with rosacea treated superficially: I would expect significant erythema and swelling peaking within 24 hours and possibly lingering through 10 days; I would plan conservative settings and anti-inflammatory post-care.
- Example 3 — 28-year-old with darker skin undergoing shallow in-office treatment: I would predict modest swelling for 48–72 hours and emphasize strict sun avoidance and inflammatory control to prevent PIH.
I use case examples to make abstract timelines more concrete.
Final considerations and takeaways
I want to leave you with clear, actionable guidance that I would follow or recommend professionally.
- Expect swelling: Swelling is a normal, transient response to microneedling and usually peaks within 24–48 hours for most skin types.
- Skin-type variability matters: Sensitive, rosacea-prone, and inflammatory-skin types often have longer or stronger swelling responses and may need conservative treatment plans.
- Management works: Simple measures—cooling, elevation, gentle hydrating products, and sun protection—can substantially reduce both the intensity and the duration of swelling.
- Safety first: If you have significant dermatologic conditions or are on medications like isotretinoin or anticoagulants, consult a dermatologist before undergoing microneedling.
- When in doubt, seek care: Infection or severe allergic reactions are rare but require prompt professional attention.
I remain available to help interpret your specific situation or to tailor aftercare plans based on your particular skin type and the exact microneedling procedure you are considering.