Have you ever wondered whether microneedling could actually make melasma worse instead of better?
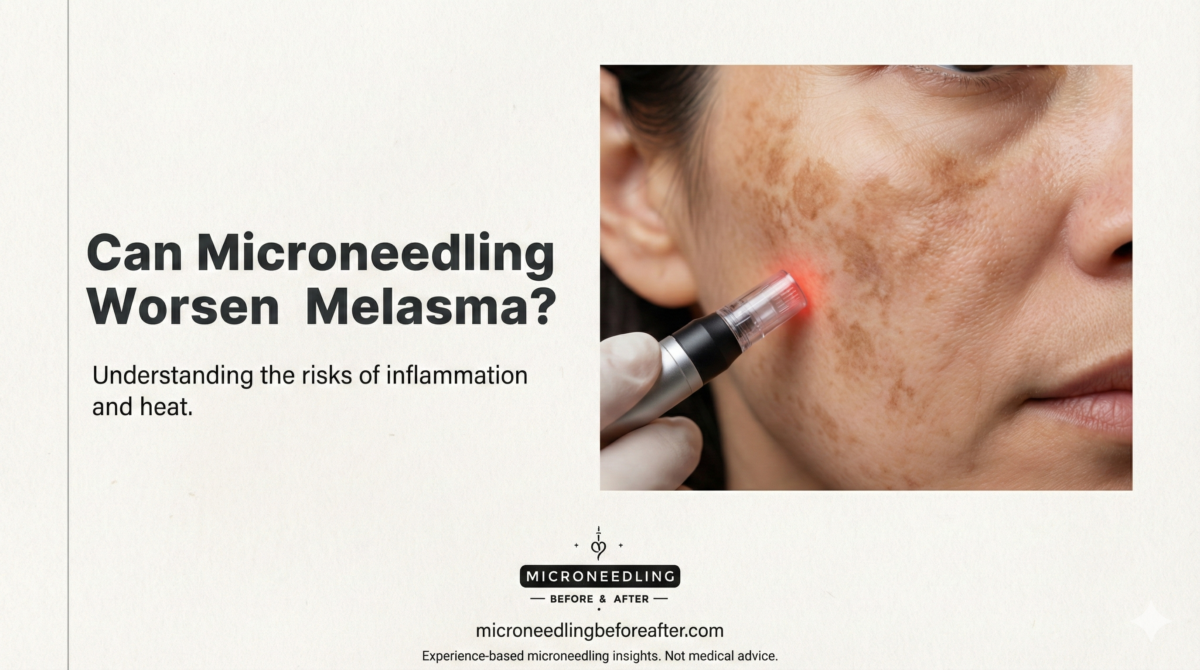
Can Microneedling Worsen Melasma
I’ll give you a clear, practical look at the question, because I know how frustrating melasma can be and how tempting microneedling sounds as a treatment option. I’ll cover mechanisms, risks, evidence, how I would approach it, and safer alternatives so you can make an informed choice.
Short answer
Yes — microneedling can worsen melasma in some situations, especially if it triggers inflammation, is performed with overly aggressive settings, or isn’t paired with proper pre- and post-procedure care. However, under controlled conditions and combined with the right topical or procedural adjuncts, microneedling may also help certain patients. I always emphasize individualized assessment and conservative technique.
What is melasma?
Melasma is a common chronic skin condition characterized by brown to gray-brown patches, typically on the cheeks, forehead, upper lip, and chin. I think of it as a pigmentary disorder driven by a combination of genetic predisposition, hormonal influences (like pregnancy or oral contraceptives), ultraviolet (UV) exposure, and other triggers such as inflammation or heat.
Melasma isn’t just “too much pigment” — its biology involves pigment-producing cells (melanocytes), the surrounding skin environment (inflammation, blood vessels), and the skin’s response to triggers. Because of that complexity, treatments that only affect one part of the process sometimes fail or can worsen the condition.
What is microneedling?
Microneedling is a minimally invasive procedure that uses tiny needles to create controlled micro-injuries in the skin. I describe it as a way to stimulate the skin’s natural repair mechanisms: increased collagen production, enhanced penetration of topical agents, and release of growth factors.
There are different devices and techniques: home-use rollers, professional pens, radiofrequency microneedling (RF), and different needle depths. The intensity and device choice matter a great deal for safety and outcomes.
How microneedling might affect melasma
I like to break this into two opposite potential effects: therapeutic and harmful.
- Therapeutic potential: Microneedling can enhance delivery of pigment-lightening topical agents and stimulate remodeling of the dermal-epidermal unit. This might help some aspects of melasma, particularly when combined with targeted therapies.
- Harmful potential: Microneedling causes inflammation. For people prone to post-inflammatory hyperpigmentation (PIH) — especially those with darker skin types — that inflammation can induce more pigment, sometimes worsening melasma rather than improving it.
Post-inflammatory hyperpigmentation (PIH) risk
One of the main concerns I focus on is PIH. Any procedure that injures the skin — even superficially — can produce pigment in susceptible individuals. I’m particularly cautious when treating Fitzpatrick skin types IV–VI because their melanocytes respond more robustly to inflammation.
When microneedling is too aggressive (too deep, too frequent, or done without proper sun protection and topical control), I’ve seen patients develop surrounding hyperpigmentation or an overall darkening of melasma patches.
Depth and technique matter
Needle length, treatment frequency, and device type are key. Superficial microneedling (around 0.25–0.5 mm) primarily improves topical penetration and causes minimal inflammation. Deeper needling (1.0 mm and above) provokes more intense remodeling and a stronger inflammatory response.
I generally recommend starting conservatively, especially for melasma. An experienced provider using a microneedling pen with controlled depth and sterile technique is preferable to home rollers or overaggressive settings.
Evidence from studies and clinical experience
The literature is mixed. I’ll summarize the general themes I’ve seen in studies and clinical reports rather than listing specific trials.
- Some clinical reports and small studies show improvement in melasma when microneedling is combined with topical agents (for example, tranexamic acid, hydroquinone, or customized serums). Enhanced penetration appears to boost effectiveness.
- Other reports describe cases of PIH or worsening pigment following microneedling, particularly when performed aggressively or without preconditioning.
- Radiofrequency microneedling (RF) introduces heat plus needling, which may increase risk of inflammation and PIH in susceptible people, although some protocols claim benefits when paired with appropriate precautions.
Overall, the evidence suggests that microneedling isn’t a one-size-fits-all solution for melasma. It can help in selected situations but can also worsen pigment if not done carefully.
When microneedling may help melasma
I consider microneedling when:
- The patient has been carefully assessed and other first-line therapies (topical agents, strict sun protection, and medication) have been optimized without sufficient improvement.
- The practitioner plans to use conservative needle depths and spacing between sessions.
- Microneedling is being used to enhance penetration of safe and effective topical therapies (for example, tranexamic acid or topical retinoids under supervision).
- The patient accepts the small but real risk of PIH and follows pre- and post-procedure instructions (sun avoidance, strict sunscreen, anti-inflammatory strategies).
When used judiciously, especially as an adjunct to other evidence-based treatments, microneedling can sometimes produce additional improvement.
When microneedling may worsen melasma
I would avoid or be very cautious with microneedling when:
- The patient has Fitzpatrick skin type IV–VI and a strong history of PIH.
- There is active inflammation, a recent sunburn, or recent acne flares in the treatment area.
- The procedure will use deep needle lengths (>1.0 mm) or aggressive protocols without preconditioning.
- The patient cannot adhere to strict post-treatment sun protection or appropriate topical management.
- Microneedling is performed by someone without experience in treating pigmentary disorders.
If I suspect a high risk of PIH, I usually recommend alternative treatments or a test patch before committing to full-face sessions.
Practical table: factors that increase or decrease risk
| Factor | Effect on Risk of Worsening Melasma | Why I Care |
|---|---|---|
| Fitzpatrick skin type IV–VI | Increases risk | More reactive melanocytes → higher PIH risk |
| Needle depth > 1.0 mm | Increases risk | Greater inflammation and injury |
| Frequency (sessions |