¿Alguna vez te has preguntado por qué mis sesiones de microagujas en casa no me dieron los resultados espectaculares que esperaba?
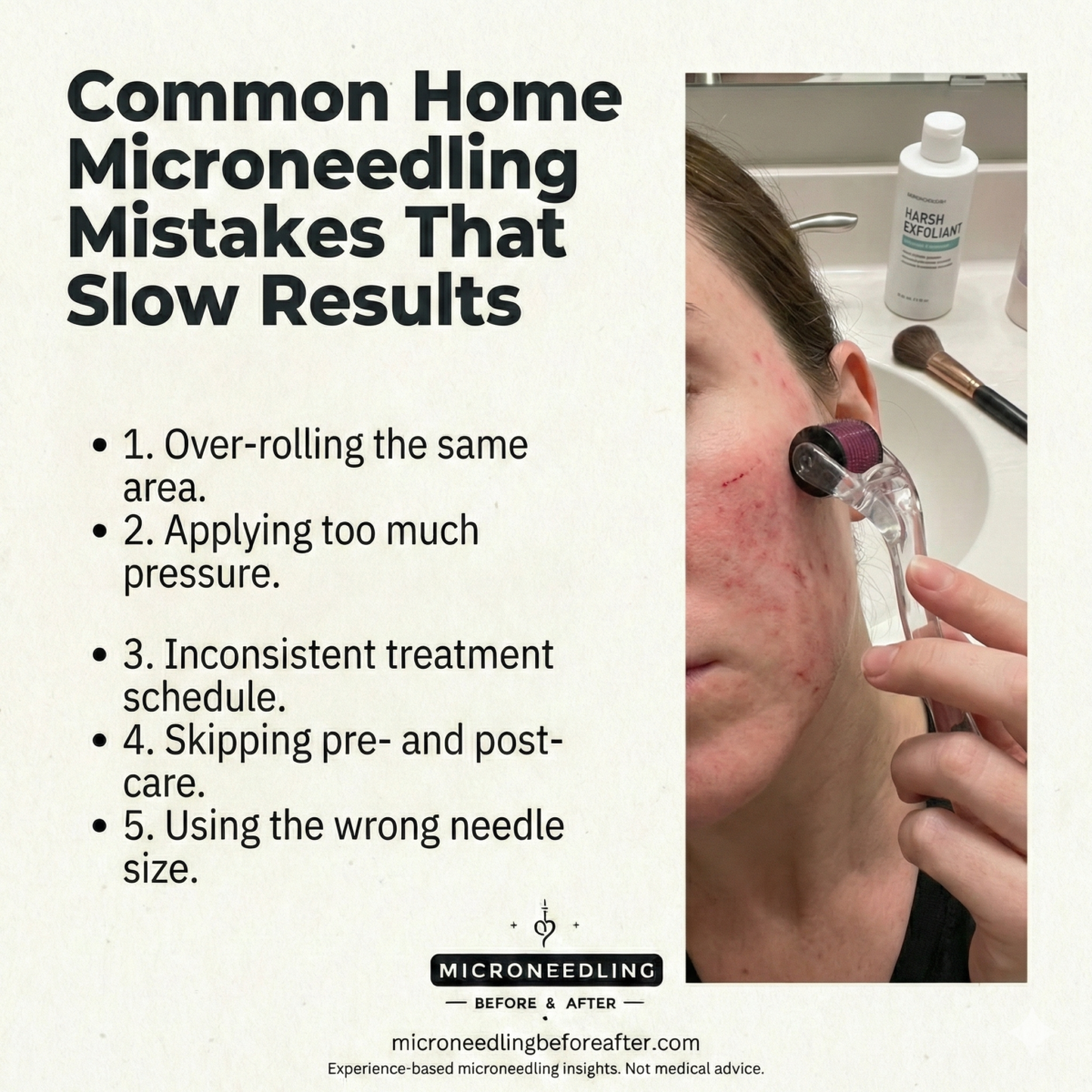
Errores comunes de microagujas en casa que retrasan los resultados
Escribí esto para compartir los errores que he visto y cometido, y las soluciones sencillas que realmente aceleran el progreso visible. La microaguja puede ser eficaz si se realiza correctamente, pero pequeños errores en casa suelen costar semanas o meses de progreso, y a veces causan contratiempos.
Qué hace la microaguja y por qué es importante la técnica
Comenzaré con una breve introducción: la microaguja utiliza agujas diminutas para crear microlesiones controladas en la piel, lo que estimula la cicatrización de la herida y la producción de nuevo colágeno y elastina. Dado que el proceso se basa en una cascada de reparación biológica, la técnica, el tiempo, la higiene y el cuidado posterior determinan la eficacia y la rapidez con la que se afianzan esos cambios.
¿Qué tan rápido debo esperar resultados?
Me gusta establecer plazos realistas para no desanimarme. Suelo decirles que esperen mejoras sutiles en 2 a 4 semanas y cambios más notables en la textura y la firmeza después de 3 meses, ya que la remodelación del colágeno lleva tiempo. Si no veo ningún cambio después de varios meses, es señal de que algo en mi rutina no va bien.
Los errores más comunes que retrasan los resultados
Analizaré en detalle los errores típicos, explicaré por qué son importantes y brindaré soluciones prácticas que he utilizado o recomendado.
Utilizando una longitud de aguja incorrecta
Mucha gente piensa que las agujas más largas dan resultados más rápidos. Yo también lo pensaba. La longitud de la aguja debe ser acorde con el problema de la piel: agujas más cortas para problemas superficiales y más largas para cicatrices o arrugas más profundas. Usar agujas demasiado cortas no activará la respuesta de colágeno; las agujas demasiado largas aumentan el riesgo de sangrado, cicatrices e infección.
- Solución: Sigue una guía de longitud de aguja según tu objetivo (ver tabla a continuación). Si no estoy segura, empiezo con una medida conservadora y consulto con un profesional para longitudes más largas.
| Longitud de la aguja (mm) | Uso típico | Riesgo si se hace un mal uso |
|---|---|---|
| 0,25 milímetros | Aumenta la absorción del producto, textura superficial. | Estimulación mínima del colágeno si se usa en exceso |
| 0,5 milímetros | Líneas finas, problemas leves de textura. | Seguro en casa con la preparación adecuada |
| 0,75–1,0 mm | Textura más profunda, cicatrices leves. | Más molestias; considere consejo profesional para >0,75 |
| 1,5 milímetros | Cicatrices moderadas y estrías | Generalmente es mejor dejarlo en manos de profesionales. |
| >1,5 mm | Cicatrices profundas e indicaciones médicas | Mayor riesgo; se recomienda un entorno profesional. |
Ir con demasiada frecuencia o no espaciar las sesiones correctamente
He visto a gente que se aplica microagujas cada pocos días con la esperanza de acelerar los resultados, lo que en realidad dificulta el progreso. La formación de colágeno requiere tiempo; las sesiones apresuradas solo irritan la piel repetidamente e impiden una curación adecuada.
- Solución: Para inyecciones de 0,25 a 0,5 mm, suelo recomendar cada 1 a 3 semanas; para inyecciones de 0,75 a 1,0 mm, cada 4 a 6 semanas; las agujas más largas requieren una recuperación más larga. Registramos las sesiones en mi calendario para evitar excederme.
Aplicar principios activos fuertes inmediatamente después de la punción.
Cuando la piel se trata recientemente con agujas, es más permeable. Esto es útil para hidratar los péptidos y el ácido hialurónico, pero potencialmente peligroso para los activos agresivos como los retinoides, los ácidos o la vitamina C de alta potencia. Aprendí a las malas que aplicarlos justo después del tratamiento causa escozor, inflamación o incluso quemaduras químicas.
- Solución: Uso sérums suaves y estériles de ácido hialurónico y péptidos calmantes después del tratamiento. Evito los retinoides y los ácidos exfoliantes durante al menos 3 a 7 días, dependiendo de la longitud de la aguja y la sensibilidad de la piel.
Saneamiento deficiente y reutilización de herramientas desechables
Las infecciones son una de las maneras más rápidas de frenar el progreso. Al principio, subestimé el riesgo de gérmenes. Los rodillos, bolígrafos o manos sucias pueden introducir bacterias en los microcanales, causando enrojecimiento prolongado, pústulas o cicatrices que pueden retrasarme meses.
- Solución: Solo uso agujas desechables o sistemas de cartuchos estériles diseñados para plumas. Desinfecto correctamente las herramientas no desechables, sigo las instrucciones del fabricante y siempre me lavo las manos y la cara antes del tratamiento.
No preparar la piel adecuadamente
Saltarme una limpieza profunda o hacerme la microaguja con restos de maquillaje o protector solar significa que estoy introduciendo contaminantes en la piel. Antes me apresuraba en este paso y lo pagaba con irritación.
- Solución: Me limpio la piel dos veces (con aceite si es necesario, luego con una espuma suave o micelar) y, si pienso usar crema anestésica, la aplico sobre la piel limpia y seca. También evito los tónicos con alcohol justo antes de la punción para evitar irritación adicional.
Saltarse una prueba de parche para nuevos sueros o dispositivos
Aprendí que las alergias y las sensibilidades a veces solo aparecen cuando la piel está dañada. Una vez, probar un nuevo sérum inmediatamente después de la punción me causó enrojecimiento y picazón intensos.
- Solución: Siempre hago una prueba localizada en la parte interna del antebrazo y espero de 24 a 48 horas. Con un dispositivo nuevo, pruebo en una pequeña zona de la mandíbula o el antebrazo para evaluar la reacción antes de tratar todo el rostro.
Técnica incorrecta: demasiados pases o dirección incorrecta
La técnica afecta tanto la seguridad como la eficacia. Solía cometer el error de repasar repetidamente la misma zona o cambiar de ángulo aleatoriamente, lo que provocaba mayor inflamación y resultados desiguales.
- Solución: Utilizo un patrón metódico (horizontal, vertical y diagonal) y limito las pasadas por zona (normalmente de 2 a 4 por dirección). Mantengo una presión constante y evito trabajar demasiado una zona de piel.
Sobreestimar los beneficios para ciertos tipos o condiciones de piel
La microaguja no es la panacea. Una vez pensé que borraría las cicatrices profundas del acné de la noche a la mañana. Esa mentalidad me llevó a la decepción. Algunas afecciones, como el acné activo, ciertas enfermedades inflamatorias de la piel o la propensión a los queloides, están contraindicadas o requieren supervisión profesional.
- Solución: Consulto a un dermatólogo en caso de cicatrices graves, rosácea activa o acné inflamatorio. Evito aplicar punción sobre lesiones activas y pospongo el tratamiento hasta que la piel se calme.
No controlar la exposición al sol y el FPS
El daño solar y la inflamación, en conjunto, intensifican la pigmentación y retrasan la cicatrización. Si me aplico microagujas y no protejo mi piel, puedo observar hiperpigmentación o enrojecimiento prolongado.
- Solución: Evito la exposición solar directa durante al menos 48 a 72 horas después del tratamiento y uso protector solar de amplio espectro con FPS 30+ a diario. Uso sombrero y gafas de sol cuando salgo al exterior.
Utilizar dispositivos de mala calidad o no regulados
He aprendido que los rodillos y bolígrafos más baratos y de baja calidad pueden tener agujas irregulares que rasgan la piel en lugar de crear microcanales limpios. Esto provoca más trauma y una recuperación más lenta.
- Solución: Compro dispositivos de marcas reconocidas que ofrecen cartuchos esterilizados de grado médico. Leo reseñas y compruebo la autorización CE/FDA cuando corresponde.
Mal uso de la crema anestésica
Las cremas anestésicas pueden ser útiles para aliviar el dolor, pero su uso inadecuado (demasiado espeso, demasiado tiempo o en zonas extensas) puede causar irritación o problemas de absorción sistémica. Una vez me dejé la crema anestésica puesta demasiado tiempo y se me enrojeció e hinchó la cara.
- Solución: sigo el tiempo de aplicación recomendado, uso el porcentaje correcto de ingrediente y evito la oclusión que aumenta la absorción a menos que lo indique un profesional.
Ignorar las señales de inflamación posteriores a la punción
Se espera algo de inflamación, pero la hinchazón persistente, el calor, el pus o el aumento del dolor sugieren una infección o una reacción adversa. Solía restarle importancia al enrojecimiento prolongado y solo después me di cuenta de que era más grave.
- Solución: Vigilo de cerca los síntomas durante 48 a 72 horas. Si empeoran o no mejoran, contacto con un profesional de la salud de inmediato.
Mezclar tratamientos de forma inadecuada (peelings químicos, depilación con cera, láser)
Combinar la microaguja con otros tratamientos fuertes demasiado pronto puede aumentar la irritación y el daño. En una ocasión, incorporé una exfoliación química a mi rutina sin el espaciamiento adecuado, lo que generó una inflamación excesiva que ralentizó los resultados.
- Solución: Espacio los tratamientos agresivos. Normalmente, dejo pasar al menos dos semanas después de una exfoliación o láser antes de aplicar la punción, pero sigo las instrucciones específicas del dispositivo y del tratamiento y hablo con el médico si tengo dudas.
Esperando milagros inmediatos de colágeno
La gente suele esperar transformaciones de la noche a la mañana. He escuchado muchas veces "Lo hice una vez y no pasó nada". La remodelación del colágeno es lenta y acumulativa; una sola sesión rara vez produce un cambio drástico a menos que se trate de un tratamiento profesional más profundo.
- Solución: Establezco un plan realista: tratamientos constantes y espaciados con un buen cuidado posterior. Hago un seguimiento del progreso con fotos cada 2 a 4 semanas para poder ver mejoras sutiles.
No adaptar el cuidado posterior a la profundidad de la aguja
El cuidado posterior de una sesión de 0,25 mm es diferente al de una de 1,0 mm. Antes, trataba todas las sesiones por igual, lo que provocaba irritación innecesaria después de tratamientos más profundos.
- Solución: para sesiones superficiales, uso hidratación suave y FPS; para sesiones más profundas, extiendo las medidas de recuperación, evito los ingredientes activos por más tiempo y priorizo el descanso y la reparación de la barrera.
Microagujas sobre infecciones activas o heridas abiertas
Este es un error innegable. Agitar sobre herpes labial, infecciones bacterianas o acné inflamado impulsa los patógenos a una mayor profundidad y corre el riesgo de propagarse.
- Solución: retraso los tratamientos hasta que las lesiones estén completamente curadas y, a veces, utilizo primero un tratamiento antiviral o antibacteriano si es necesario.
¿Es la microaguja mejor que el masaje facial para el colágeno?
Me preguntan esto mucho, así que seré directo: la microaguja y el masaje facial funcionan de manera diferente, y “mejor” depende del objetivo.
- La microaguja crea microlesiones controladas que estimulan directamente la cascada de cicatrización, lo que resulta en un aumento de colágeno y elastina en la dermis. Para una inducción de colágeno medible, especialmente al tratar cicatrices, texturas profundas o laxitud significativa, la microaguja es más efectiva que el masaje.
- El masaje facial mejora la circulación, el drenaje linfático y el tono muscular, y puede rellenar temporalmente la piel al aumentar el flujo sanguíneo y de líquidos. Con el tiempo, puede contribuir a una piel de aspecto más saludable y a mantener el colágeno, pero no produce el mismo grado de remodelación del colágeno que la microaguja.
Me gusta pensarlo así: si mi objetivo es modificar la estructura del colágeno para cicatrices o arrugas, elijo la microaguja. Si mi objetivo es una luminosidad inmediata, relajación o favorecer el flujo linfático, el masaje es una herramienta excelente. Combinar ambas —la microaguja para remodelar y el masaje para el mantenimiento y la circulación— suele dar los resultados más equilibrados.
Aquí hay una tabla de comparación rápida que uso para explicar las diferencias:
| Factor | Microagujas | Masaje facial |
|---|---|---|
| Mecanismo primario | Microlesión → remodelación del colágeno | Estimulación mecánica → circulación y flujo linfático |
| Inducción de colágeno | Alto (especialmente con la profundidad adecuada) | Bajo a moderado (mantenimiento) |
| Resultados inmediatos | Enrojecimiento e hinchazón; textura/firmeza a largo plazo | Brillo instantáneo y reducción de la hinchazón. |
| Falta del tiempo | 24 horas a varios días (dependiendo de la profundidad) | Mínimo o ninguno |
| Riesgo | Infección y cicatrices si se usa mal | Bajo (posibles hematomas) |
| Mejor para | Cicatrices, arrugas profundas, laxitud. | Relajación, circulación y volumen temporal. |
Guía de longitud de aguja y cuándo consultar a un profesional
Ya he mencionado algunas longitudes, pero aquí hay un desglose más claro que sigo, con orientación sobre cuándo buscar ayuda profesional.
Mis recomendaciones sobre la longitud de las agujas y su justificación
Considero que esta tabla es útil para compartir con amigos o clientes que preguntan qué pueden hacer de manera segura en casa frente a cuándo acudir a una clínica.
| Longitud de la aguja | ¿Usar en casa? | Uso típico | Cuándo consultar a un profesional |
|---|---|---|---|
| 0,25 milímetros | Sí | Absorción del producto, textura suave. | El uso doméstico está bien |
| 0,5 milímetros | Sí | Líneas finas, cicatrices leves | Uso doméstico aceptable con precaución |
| 0,75 milímetros | Sí para usuarios experimentados | Cicatrices moderadas, líneas más profundas | Considere un profesional si no está seguro |
| 1,0 milímetros | Precaución | Cicatrices más profundas, remodelación más significativa | Suelo recomendar sesiones profesionales. |
| 1,5 mm y más | No | Cicatrices importantes, estrías | Solo para profesionales |
Lista de verificación de cuidados posteriores que utilizo siempre
Mantengo una lista de verificación sencilla para minimizar errores y optimizar resultados. Puedes copiarla para tu propia rutina.
- Limpie completamente antes del tratamiento (limpieza doble si es necesario).
- Utilice un dispositivo/cartucho estéril y manos limpias.
- Limitar a pases y direcciones recomendados.
- Post-tratamiento: aplicar un serum suave y estéril de ácido hialurónico o de péptidos.
- Evite los retinoides y ácidos durante 3 a 7 días (más tiempo para una punción más profunda).
- Mantener alejado del sol y utilizar protección solar FPS 30+ diariamente.
- Evite los entrenamientos intensos, las saunas y la natación durante 48 a 72 horas.
- No se toque, rasque ni exfolie hasta que la piel esté completamente curada.
- Vigile si hay signos de infección y comuníquese con un proveedor si los hay.
Solución de problemas de resultados lentos o deficientes
Si mi progreso se estanca, reviso esta lista de verificación:
- ¿Estoy usando la longitud y frecuencia de aguja correctas?
- ¿Mis herramientas están esterilizadas y en buen estado?
- ¿Tengo una técnica constante y suave (sin trabajar demasiado la piel)?
- ¿Se están aplicando los ingredientes activos demasiado pronto o con demasiada frecuencia?
- ¿Estoy protegiendo la piel de la exposición al sol?
- ¿Tengo una condición subyacente (acné activo, rosácea, pigmentación) que requiere orientación médica?
- ¿He realizado un seguimiento de los resultados con fotografías para medir el cambio objetivamente?
Si varias respuestas son "no", las corrijo y espero el tiempo necesario antes de continuar. Si las respuestas son "sí" y después de varios meses siguen sin obtener resultados, consulto con un dermatólogo para una evaluación profesional y la posibilidad de microagujas o terapias complementarias en la clínica.
Combinando la microaguja con activos tópicos de forma responsable
Me encanta la idea de mejorar la penetración, pero es fundamental tener cuidado. Suelo usar sérums de bajo riesgo, como ácido hialurónico, péptidos o sérums con factores de crecimiento, después del tratamiento. Es necesario reintroducir vitamina C de alta concentración, retinoides potentes o ácidos AHA/BHA más adelante, una vez que la barrera se haya recuperado.
- Secuencia práctica que sigo: Inmediatamente después: suero hidratante calmante estéril. Entre 24 y 72 horas después: productos suaves. Después de una semana completa (más tiempo para tratamientos más profundos), reanudar los activos gradualmente, prestando atención a la sensibilidad.
Cuándo detenerse y buscar ayuda médica
Siempre les digo a las personas, y me lo recuerdo a mí misma, que el empeoramiento de los síntomas requiere atención profesional. Si veo enrojecimiento que se extiende, dolor intenso, fiebre, pus o cualquier signo de que la piel no cicatriza, dejo el autotratamiento y contacto con un médico. La intervención temprana previene daños a largo plazo.
Expectativas realistas y estrategia a largo plazo
La microaguja es más efectiva como parte de un plan continuo. Me comprometo a realizar una serie de tratamientos, con el intervalo adecuado, a la vez que cuido la piel a diario: protector solar, un limpiador suave, hidratantes que fortalezcan la barrera cutánea y activos específicos, aplicados con prudencia.
También recomiendo hacer un seguimiento del progreso con fotos estandarizadas y notas sobre la configuración del dispositivo, los sueros utilizados y los posibles efectos secundarios. Así puedo identificar qué funciona y qué no.
Preguntas frecuentes que me hacen mucho
Responderé brevemente algunas preguntas comunes, tal como suelo explicarlas a mis amigos.
¿Cuántas sesiones necesitaré para ver resultados significativos?
Normalmente recomiendo al menos de 3 a 6 sesiones con un intervalo adecuado, con tratamientos de mantenimiento posteriores. Algunas mejoras aparecen antes, pero los cambios estructurales del colágeno requieren múltiples tratamientos y tiempo.
¿Puedo usar retinol entre sesiones?
Evito el retinol durante varios días después del tratamiento (de 3 a 7 días, dependiendo de la intensidad). Entre sesiones, reintroduzco el retinol gradualmente si mi piel lo tolera, pero nunca aplico capas de retinoides fuertes inmediatamente después de la punción.
¿La microaguja es dolorosa?
El dolor varía. Las agujas de 0,25 a 0,5 mm suelen ser tolerables sin anestesia; las agujas más largas son más incómodas y podrían beneficiarse de la anestesia tópica. Considero prioritaria la comodidad frente a la seguridad y sigo los protocolos de anestesia recomendados si las utilizo.
¿La microaguja puede causar hiperpigmentación?
Sí, si no se realiza correctamente o si no protejo la piel de la exposición solar posteriormente. Las personas con tonos de piel más oscuros deben ser especialmente cautelosas y, a menudo, se benefician de la orientación profesional para minimizar la hiperpigmentación postinflamatoria.
¿Son los rodillos derma tan buenos como los bolígrafos de microagujas?
Los dermapens con cartuchos desechables suelen ser más seguros y ofrecen una penetración de la aguja más uniforme. Evito los rodillos tradicionales para las zonas faciales porque pueden dañar la piel de forma desigual y son más difíciles de esterilizar.
Reflexiones finales y mis mejores consejos
Terminaré con los consejos prácticos y fáciles de recordar que yo mismo utilizo:
- Comience de forma conservadora con la longitud y frecuencia de la aguja.
- Priorizar la higiene y los dispositivos estériles.
- Utilice sueros suaves e hidratantes inmediatamente después del tratamiento.
- Protege tu piel del sol y evita los activos agresivos durante un periodo apropiado.
- Realice un seguimiento de las sesiones y los resultados con fotografías.
- No tenga miedo de pedir ayuda a un profesional si tiene cicatrices importantes, una enfermedad cutánea activa o reacciones inusuales.
Si sigo estas pautas, reduzco la posibilidad de obtener resultados lentos o estancados y aprovecho cada sesión. La microaguja puede ser una herramienta muy eficaz si se trata con respeto, paciencia y constancia.