?Which one will actually make my skin look and feel better: microneedling or slathering on a topical collagen product?
Microneedling Vs Topical Collagen Products
I get asked this question a lot, and I want to walk through the science, the practical differences, and how to choose based on real goals. I’ll share what I’ve learned from research, clinical experience, and practical considerations so you can make an informed choice.
What are microneedling and topical collagen products?
I like to start with basic definitions so we’re on the same page. Microneedling is a procedure that uses tiny needles to create micro-injuries in the skin, triggering a wound-healing response that stimulates collagen and elastin production. Topical collagen products are creams, serums, or masks that contain collagen molecules (or ingredients aimed at supporting collagen) and are applied to the skin to provide hydration, texture improvements, or a collagen “boost.”
Microneedling: definition and mechanism
I describe microneedling as a controlled way to tell the skin to repair itself. By creating microchannels, the procedure activates inflammatory and repair pathways, increases growth factor release, and can improve skin thickness and texture over time.
Topical collagen products: definition and mechanism
When I talk about topical collagen, I refer to formulations containing collagen (native or hydrolyzed), peptides, or collagen-supporting ingredients. These products primarily act on the surface — they hydrate, temporarily fill fine lines, and may provide topical peptides that signal cells to maintain or synthesize collagen, but intact collagen molecules are typically too large to deeply penetrate intact skin.
How they work: biology and skin response
I find the difference in mechanism is the most important concept to understand. Microneedling leverages the skin’s repair mechanisms to stimulate new collagen internally, whereas topical collagen products largely act externally and signal support.
Microneedling: wound healing and collagen induction
I think of microneedling as a stimulus that recruits platelets, macrophages, and fibroblasts, releasing growth factors like TGF-β, PDGF, and VEGF. These signals encourage fibroblasts to lay down new collagen types I and III and remodel the extracellular matrix, improving skin tone, scars, and elasticity over repeated treatments.
Topical collagen: absorption and limitations
I always explain that intact collagen molecules are large; they mostly sit on the skin surface and act as humectants and occlusives. Hydrolyzed collagen and certain peptides are smaller, and they can act as signals or provide amino acids, but they typically do not rebuild the deeper dermal collagen matrix the way an induced wound-healing response can.
Evidence and effectiveness
I like to separate clinical evidence for each option so readers know what’s backed by studies vs anecdote. Microneedling has a stronger clinical evidence base for improving scars, fine lines, and skin texture than most topical collagen products.
Clinical studies on microneedling
I review randomized controlled trials and observational studies and see consistent improvements in acne scarring, fine lines, and skin thickness after multiple sessions of microneedling. I note that outcomes improve with session number and proper device parameters, and that histologic studies show increased collagen deposition after treatment.
Clinical studies on topical collagen
I acknowledge that topical collagen products have shown benefits for hydration, surface smoothness, and transient plumping in controlled studies. I also point out that evidence for deep structural changes in dermal collagen from topical collagen alone is limited, and many product claims overstate penetrative effects.
Head-to-head research
I don’t see many high-quality head-to-head trials comparing microneedling directly with topical collagen products, because they’re fundamentally different interventions. Where combination studies exist, microneedling plus topical agents often outperforms topical agents alone, particularly for scar remodeling and visible texture improvements.
Benefits and limitations
I usually list benefits and limitations side by side so readers can weigh trade-offs. Both approaches have meaningful roles depending on the goal, timeline, budget, and risk tolerance.
Benefits of microneedling
I see microneedling deliver measurable improvements in acne scars, surgical scars, laxity, and fine lines by stimulating the body’s own collagen production. I also value its versatility — it can be combined with PRP (platelet-rich plasma), topical growth factors, or performed at different needle depths for tailored outcomes.
Limitations of microneedling
I want people to remember it’s not a one-and-done fix: microneedling requires a series of treatments and some downtime, with redness and sensitivity expected for a few days. I also caution that results vary by device quality, practitioner skill, and individual healing capacity, and complications like infection or hyperpigmentation can occur if performed improperly.
Benefits of topical collagen products
I appreciate that topical collagen products are low-risk and easy to use daily; they improve hydration, reduce surface roughness, and can support skin barrier function. I also note they can boost skin comfort and appearance quickly with minimal cost and no downtime.
Limitations of topical collagen products
I always temper expectations: most topicals don’t rebuild dermal collagen in a clinically meaningful way, and product claims can be inflated. I also underline that product formulation, concentration, and adjunct ingredients determine value, and cheaper formulas often deliver little beyond basic moisturization.
Safety considerations
I emphasize safety first, because both options interact with the skin differently and carry different risk profiles. Understanding side effects, contraindications, and best practices reduces chance of harm.
Risks of microneedling
I warn that microneedling can cause bleeding, bruising, infection, scarring, and post-inflammatory hyperpigmentation if not done correctly. I recommend using sterile equipment, avoiding active infections and isotretinoin usage windows, and consulting trained professionals for deeper needling.
Risks of topical collagen products
I explain that topical collagen products are generally low risk, though they can cause irritation, allergic reactions, or acne flare in some people depending on formulation. I advise patch testing new formulas and avoiding products with irritating fragrances or comedogenic bases if you are sensitive.
Who should avoid each approach
I tell people who have active acne, open wounds, keloid tendency, or recent isotretinoin use to avoid professional microneedling until cleared by a clinician. For topical collagen, I advise caution for those with known sensitivities to marine or bovine collagen sources and suggest reading ingredient lists carefully if you have allergies.
Procedure, aftercare, and recovery
I like to walk readers through what an appointment looks like and what to do afterward, because realistic expectations matter for satisfaction.
What to expect during a microneedling session
I describe that a typical session takes 30–60 minutes and may include numbing cream before treatment, followed by device passes across treatment areas. I tell people they’ll feel tickling, pressure, or brief pricks, and that the level of discomfort depends on needle depth and device type.
Aftercare following microneedling
I always emphasize gentle care: avoid sun exposure, use broad-spectrum sunscreen, steer clear of retinoids and active acids for several days, and rely on gentle, hydrating products while the skin re-epithelializes. I also recommend following practitioner-specific instructions for cleansing, topical antibiotics if prescribed, and signs of complications to watch for.
Using topical collagen effectively
I advise applying topical collagen products to clean skin as part of a routine that includes sunscreen and supportive ingredients like hyaluronic acid and antioxidants. I recommend consistent daily use for maintenance benefits and choosing formulations that complement your skin type and other actives.
Cost and accessibility
I know cost and convenience often drive decisions as much as efficacy, so I break this down clearly. Costs vary significantly depending on whether you choose professional microneedling, at-home derma rollers, or high-end topical formulations.
Microneedling cost factors
I explain that professional microneedling treatments can range widely — from modest in-office radiofrequency-assisted options to pricier physician-performed sessions — with series pricing often needed to achieve results. I also point out that costs increase with adjuncts like PRP, topical growth factors, or advanced devices.
Topical collagen cost factors
I note that topical collagen products range from budget drugstore creams to premium serums with added peptides and growth-factor mimetics. I remind readers that higher price doesn’t always equal higher efficacy and to evaluate ingredient lists and formulations rather than price alone.
Home devices vs professional treatments
I caution that home derma rollers and motorized devices exist, but they generally use shorter needles and produce more modest results than professional tools. I advise caution with DIY deeper needling due to sterilization and technique issues; if I were to try home microneedling, I’d stay conservative and focus on surface-level devices.
Choosing the right option for you
I encourage readers to match the intervention to their goals, budget, and risk tolerance. There’s no single right answer for everyone, and sometimes a combined approach is best.
Assessing your skin goals and condition
I tell people to ask themselves whether they want hydration and minor smoothing (where topicals can help) or structural improvement for scars and laxity (where microneedling is more effective). I also recommend considering skin tone, susceptibility to hyperpigmentation, and medical history when choosing.
When to combine both approaches
I often recommend combining microneedling with targeted topicals for enhanced outcomes: microneedling can increase topical absorption immediately after treatment, but only under professional guidance to avoid irritation. I also find that ongoing topical skincare maintains and augments the benefits of procedural interventions.
Consulting a professional
I stress that consulting a dermatologist or licensed aesthetician is wise, especially for moderate-to-severe concerns, darker skin tones, or a history of keloids. I’d rather someone get a few professional opinions than attempt aggressive DIY regimens that risk harm.
Comparison table: microneedling vs topical collagen
I created a table to help visualize the differences quickly so readers can reference the most important variables. This table highlights mechanism, evidence, downtime, and ideal use cases.
| Feature | Microneedling | Topical Collagen Products |
|---|---|---|
| Mechanism | Creates micro-injuries to stimulate dermal collagen production | Applies collagen or collagen-supporting ingredients to skin surface |
| Evidence for deep remodeling | Stronger clinical evidence for scarring, texture, thickness | Limited for deep remodeling; good for hydration/surface |
| Onset of visible results | Weeks to months; improves with multiple sessions | Immediate temporary plumping; longer-term maintenance benefits |
| Downtime | Mild to moderate (redness, sensitivity for days) | Minimal to none |
| Risk profile | Higher — possible infection, hyperpigmentation, scarring | Low — irritation or allergy possible |
| Cost | Higher per session; multiple sessions often required | Varies; often lower cost and subscription-based |
| Best for | Scars, texture, fine lines, skin laxity | Hydration, barrier support, temporary smoothing |
| Suitability for home use | Professional recommended for deeper needling | Easily used at home daily |
Product selection and ingredients to look for
I want readers to know which ingredients actually matter in topical products and how they might support or fail to support collagen health. Proper formulation and complementary actives are often more important than the presence of “collagen” on a label.
What to look for in topical collagen products
I recommend checking whether the product contains hydrolyzed collagen (smaller peptides), supportive peptides, and adequate humectants like glycerin or hyaluronic acid. I also suggest looking for stable packaging, proper preservative systems, and non-irritating bases if you have sensitive skin.
Complementary ingredients that enhance results
I often favor products with vitamin C (for collagen synthesis), niacinamide (for barrier repair and pigmentation control), peptides (to signal fibroblasts), and hyaluronic acid (for hydration). I advise caution pairing strong actives immediately after procedures and consulting your clinician for optimal timing.
My personal recommendations and practical tips
I try to give actionable guidance for different scenarios, because theoretical knowledge isn’t helpful without practical steps. Below I share what I would do in common skin situations and a sample regimen to consider.
If I had to choose
If my main problem were acne scars or skin texture, I would prioritize professional microneedling performed by a trained provider and plan a series of treatments. If my primary goals were hydration and minor surface smoothing with no downtime, I’d commit to a high-quality topical regimen containing peptides, hyaluronic acid, and vitamin C.
Routine example
If I were combining approaches, I’d receive microneedling in the clinic every 4–8 weeks for several sessions, and maintain daily topical care at home with sunscreen, antioxidants in the morning, and reparative peptides and hydrators at night. I would also avoid strong exfoliants for at least a week after microneedling and use calming, barrier-supportive products.
Avoiding pitfalls
I tell people to avoid overzealous DIY needling with long needles and to be skeptical of marketing that promises dramatic collagen remodeling from a jar. I also advise consistent sunscreen use; UV exposure undermines both collagen production and results from procedures.
Frequently asked questions (FAQs)
I include FAQs because people commonly have the same practical concerns and misconceptions. Each answer is concise and rooted in current understanding.
Will topical collagen replace microneedling?
I don’t think topical collagen replaces microneedling for structural improvements. Topicals help hydrate and support the skin, but microneedling stimulates new collagen production deeper in the dermis.
Can microneedling make collagen products work better?
I believe microneedling can increase the penetration of topicals applied immediately afterwards, but this must be done under professional guidance to avoid irritation and infection. Using growth-factor serums or PRP in conjunction with microneedling is a common strategy in clinical settings.
How many microneedling treatments do I need?
I usually recommend a series of 3–6 treatments spaced 4–8 weeks apart for optimal improvement, though individual responses vary. Maintenance sessions spaced 6–12 months apart can help preserve gains.
Are at-home microneedling devices safe?
I think home devices with very short needles (0.25–0.5 mm) can be safe for enhancing topical absorption and stimulating mild exfoliation, but deeper needling should be left to professionals. Sterility, technique, and realistic expectations are key for home use.
Can topical collagen cause allergies?
Yes, I’ve seen allergic reactions in people sensitive to marine or bovine collagen sources or to fragrance and preservatives in formulations. Patch testing new products is a simple precaution I recommend.
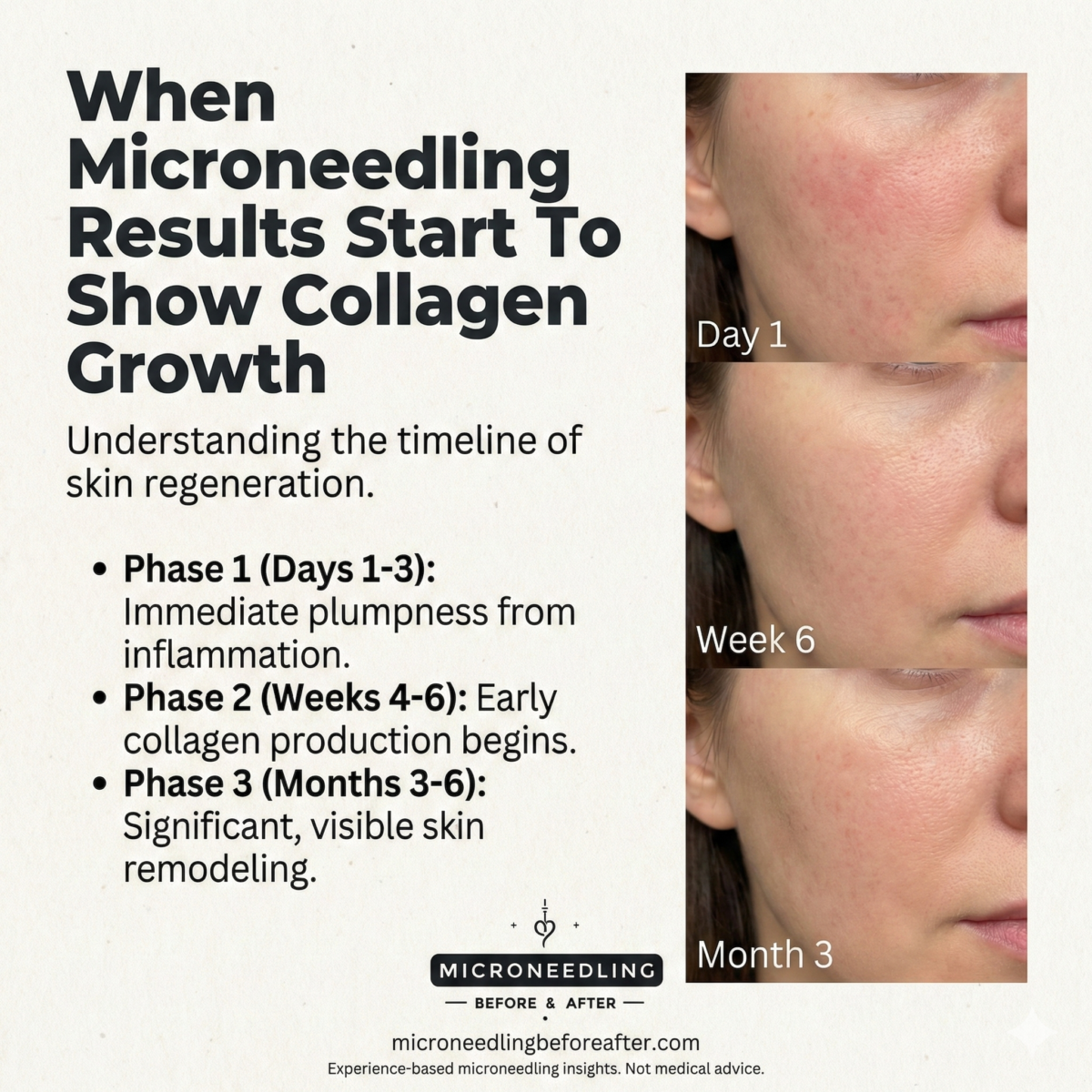
How soon will I see results?
For topical collagen, I expect immediate improvements in hydration and surface appearance, with cumulative benefits over weeks. For microneedling, visible improvements usually appear over weeks to months as collagen remodeling occurs.
Clinical scenarios and decision pathways
I offer practical decision trees for common concerns so readers can map their condition to the likely best option. These pathways reflect what I would discuss in a consultation.
Mild dehydration and fine surface lines
I’d prioritize topical collagen formulations with humectants, hyaluronic acid, antioxidants, and peptides. If results plateau, I’d consider gentle professional resurfacing or microneedling.
Acne scarring and texture irregularity
I’d recommend professional microneedling (possibly combined with PRP or laser in certain cases) as the primary modality. After an initial series, ongoing topical maintenance with peptides and sunscreen helps sustain improvements.
Skin laxity and early aging
I’d evaluate whether microneedling alone is enough or whether radiofrequency-assisted microneedling or other energy-based devices are needed for more significant tightening. Topical support remains important for skin health but is unlikely to substitute for procedural tightening when laxity is moderate.
My final thoughts
I want you to come away with a clear sense that both microneedling and topical collagen products have roles, but they are not interchangeable. Microneedling is a procedure that induces new collagen via biologic pathways and can improve scars and deeper structural issues, while topical collagen products primarily hydrate and support surface appearance with limited capacity for deep remodeling.
Summary
I encourage a pragmatic approach: define your goals, assess your risk tolerance and budget, consult a qualified professional for procedures, and use evidence-backed topical products to maintain and augment results. If I can help you think through a specific case or recommend questions to ask a clinician, I’m happy to help.