When will I start to see collagen growth after microneedling?
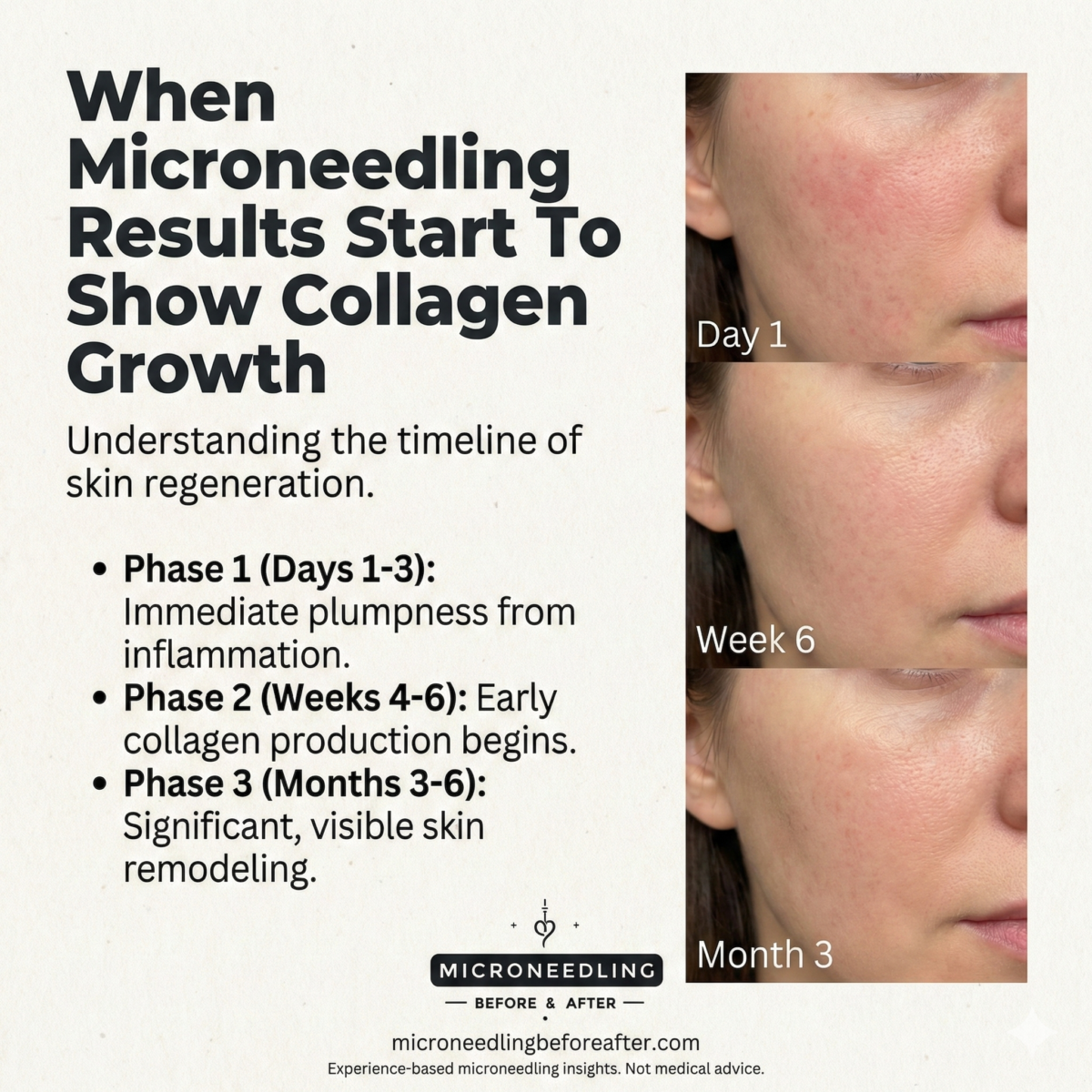
When Microneedling Results Start To Show Collagen Growth
I wrote this article to clarify the timeline and mechanisms by which microneedling triggers collagen growth. I will explain what to expect, why results vary, and how to monitor and support the process for the best clinical outcome.
What this article covers
I will outline the biological response to microneedling, provide an evidence-based timeline for collagen synthesis and visible results, and identify the variables that meaningfully alter outcomes. I will also describe monitoring techniques, appropriate aftercare, and practical recommendations to optimize collagen production safely.
How microneedling stimulates collagen production
I consider microneedling a controlled dermal injury that intentionally activates wound-healing pathways. By creating multiple microchannels in the skin, the procedure initiates an inflammatory cascade and growth factor release that ultimately stimulates fibroblasts to synthesize new collagen and extracellular matrix.
The three phases of wound healing relevant to microneedling
The wound-healing process occurs in overlapping phases: inflammation, proliferation, and remodeling. I will summarize each phase and its role in collagen synthesis so you can understand why visible changes take weeks to months.
- Inflammation: Immediately after treatment, platelets release growth factors and immune cells clear debris. I emphasize that this phase sets the stage for fibroblast activation but does not produce significant visible collagen.
- Proliferation: Fibroblasts proliferate and begin depositing type III collagen and glycosaminoglycans. I note that this phase typically spans days to weeks and is when early extracellular matrix changes occur.
- Remodeling: Type III collagen is gradually replaced with stronger type I collagen and the collagen fibers reorganize. I point out that remodeling can continue for months, which is why patients often notice progressive improvement over time.
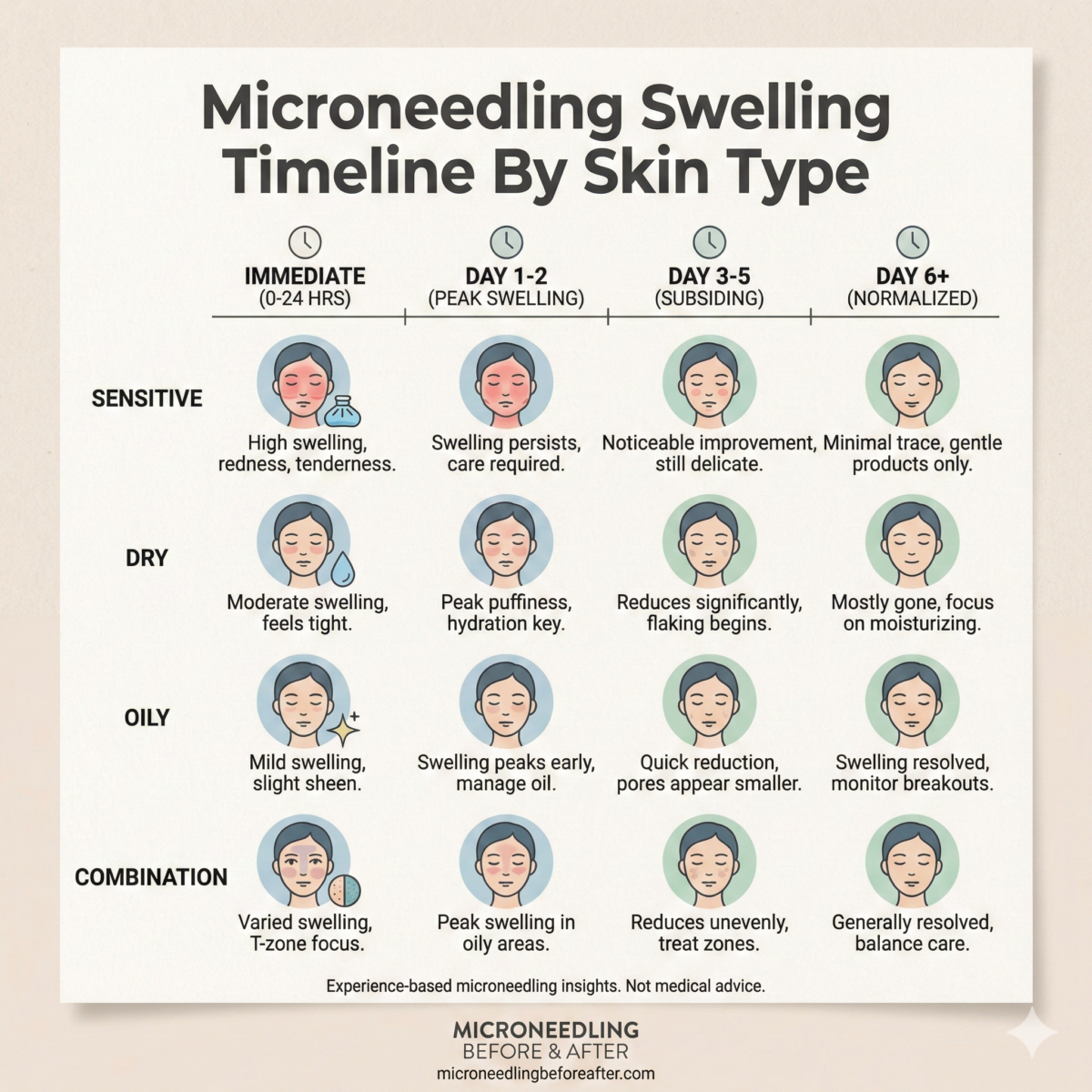
Immediate skin response and what it means
Right after microneedling I expect erythema, mild swelling, and pinpoint bleeding in some cases. These signs indicate vascular and inflammatory activation, but they are not direct evidence of new collagen formation at that moment.
The significance of erythema and microinjuries
Erythema reflects increased blood flow and inflammatory mediator release, which are necessary for healing. I emphasize that this acute response is a prerequisite for collagen synthesis but is separate from the structural collagen changes that occur later.
How early biochemical signals predict later collagen formation
Growth factors such as TGF-β, PDGF, and VEGF are upregulated within hours to days after injury. I describe that these signaling molecules recruit and activate fibroblasts, providing the biochemical environment for collagen deposition over the ensuing weeks.
Typical timeline for collagen growth after microneedling
I will present a practical timeline that clinicians and patients can use to set expectations. This timeline blends cellular biology with clinical observations from trials and practice.
Week 0–1: Immediate reaction and early signaling
During the first week, I expect acute inflammation and re-epithelialization of the epidermis. I clarify that while growth factors surge during this interval, appreciable collagen deposition has not yet occurred in amounts visible clinically.
Weeks 1–4: Early fibroblast activity and initial matrix deposition
Between one and four weeks, fibroblasts begin synthesizing collagen, primarily type III collagen, and new extracellular matrix components appear. I note that microscopic changes are underway, and some patients may notice subtle improvements in skin texture or reduced fine lines at this stage.
Weeks 4–8: Increasing collagen synthesis and early remodeling
At one to two months, I expect collagen deposition to increase and the initial remodeling of collagen fibers to start. I explain that clinical improvement becomes more noticeable for many patients during this window.
Weeks 8–12: Continued remodeling and visible aesthetic gains
From two to three months, I commonly observe measurable improvements in firmness, fine lines, and skin tone uniformity. I stress that type III collagen is transitioning to the stronger type I collagen, and the architecture of the dermal matrix becomes more organized.
3–6 months and beyond: Long-term remodeling and maximal results
I tell patients that the most durable improvements usually appear between three and six months and may continue to accrue up to a year after treatment. I emphasize that final collagen remodeling and strengthening of the dermal scaffold can take several months, which is why patience is necessary.
Timeline table: expected collagen activity and clinical signs
I include a concise table to summarize the timeline so that readers can quickly reference expected cellular events and clinical observations.
| Timeframe | Cellular events | Clinical signs I might observe |
|---|---|---|
| Immediate (0–7 days) | Hemostasis, platelet activation, growth factor release | Erythema, swelling, crusting, minimal visible collagen |
| Early (1–4 weeks) | Fibroblast recruitment, type III collagen deposition begins | Subtle texture improvement, decreased superficial roughness |
| Intermediate (4–8 weeks) | Increased collagen production, early remodeling | Noticeable improvement in fine lines, skin firmness starts |
| Late (8–12 weeks) | Transition from type III to type I collagen, fiber reorganization | Continued tightening, improved elasticity and tone |
| Long-term (3–12 months) | Ongoing remodeling and maturation of collagen | Maximal clinical benefit, sustained structural change |
Factors that affect how quickly collagen grows
I recognize that the timeline varies significantly among patients because of intrinsic and extrinsic factors. I will list and explain the most influential variables so you can assess realistic expectations.
Patient age and intrinsic regenerative capacity
Younger skin generally regenerates faster and produces collagen more efficiently. I explain that aging reduces fibroblast activity and stem cell responsiveness, which often lengthens the time to visible collagen-related improvements.
Skin type, ethnicity, and baseline photodamage
Different skin phototypes and degrees of photoaging influence healing and collagen response. I note that heavily photoaged skin may require more treatments and a longer remodeling period to achieve similar results to less-damaged skin.
Treatment depth and needle length
Needle depth plays a key role in the degree of dermal injury and the resulting collagen stimulus. I provide more detail in the table below because needle depth should be matched to the indication and safety profile.
| Needle depth (approx.) | Typical indication | Expected collagen response |
|---|---|---|
| 0.25–0.5 mm | Epidermal issues, product absorption | Minimal dermal collagen stimulation; enhanced topical penetration |
| 0.5–1.0 mm | Fine lines, superficial scarring | Moderate fibroblast activation and collagen deposition |
| 1.0–2.5 mm | Deep acne scars, laxity | Robust dermal injury with stronger collagen stimulation; more downtime |
| >2.5 mm (rare) | Specialist procedures | Higher risk; significant collagen induction but needs expertise |
I advise that increasing depth typically yields stronger collagen stimulus but also increases risk and recovery time. I stress that professional judgment must guide depth selection.
Number of passes, device type, and technique
The total energy delivered—combination of needle depth, number of passes, and cadence—affects the collagen response. I indicate that consistent, controlled techniques performed by trained providers produce more reproducible outcomes than aggressive, uncontrolled treatments.
Treatment frequency and cumulative sessions
Collagen synthesis is cumulative; multiple treatments spaced appropriately often yield superior outcomes. I usually recommend a series of three to six treatments at 4–6 week intervals for many indications, while tailoring the plan to the individual’s response.
Adjunctive therapies and combination treatments
Using growth factors, platelet-rich plasma (PRP), topical vitamin C, or lasers in concert with microneedling can amplify collagen production. I caution that combination strategies must be evidence-based and timed correctly to avoid overstimulation or increased risk of adverse effects.
Lifestyle and systemic health
Nutrition, smoking status, sun exposure, sleep, and systemic conditions (e.g., diabetes, autoimmune disease) influence wound healing and collagen synthesis. I consistently counsel patients that optimizing systemic health improves outcomes and shortens recovery.
Clinical evidence: what trials show about timing of collagen changes
I will summarize key findings from published studies so readers can see how controlled research aligns with clinical experience. I emphasize both histologic and clinical endpoints.
Histologic findings from representative studies
Several histologic studies demonstrate increased collagen deposition as early as 4 weeks post-treatment, with more pronounced and mature collagen forms by 12 weeks. I note that biopsies commonly show increased collagen content, fibroblast proliferation, and neovascularization at these time points.
Clinical outcomes and patient-reported timelines
Clinical studies frequently report noticeable improvements in texture and scarring within 1–3 months, with continued improvements up to 6 months. I point out that patient satisfaction typically correlates with the cumulative number of sessions and realistic preoperative counseling.
Monitoring collagen growth: objective and subjective measures
I recommend a combination of objective measurements and patient-reported outcomes to evaluate progress. I explain practical methods that clinicians and patients can use to track changes.
Imaging and biophysical tools
High-frequency ultrasound, optical coherence tomography (OCT), and cutometer measurements can quantify increases in dermal thickness and elasticity. I advise that while these tools are useful in research and specialty clinics, they may not be readily available in all practices.
Standardized photography and clinical grading scales
Standardized photography under consistent lighting, angles, and positioning is a reliable way to document visible improvements. I often use validated scar and wrinkle grading scales to provide objective comparisons across timepoints.
Patient-reported outcomes and tactile assessment
Patient perception of texture, tightness, and confidence are important outcomes that sometimes precede measurable structural changes. I include tactile assessment of skin firmness and palpation as practical office-based assessments that supplement imaging.
At-home microneedling devices vs professional treatments
I will contrast the stimulation and safety profiles of at-home dermal rollers and pens with in-office professional procedures. I recommend evidence-based practices to achieve results without unnecessary risk.
Comparative depth and collagen stimulation
At-home devices typically use short needles (0.2–0.5 mm) that primarily enhance topical absorption and produce minimal dermal collagen induction. I point out that professional treatments with deeper needles (1.0 mm and above) create controlled dermal injury and a stronger stimulus for collagen synthesis.
Safety, sterility, and complication risk
Professional treatments reduce infection risk and ensure appropriate technique and depth selection. I caution that improper home device use can cause infection, post-inflammatory hyperpigmentation, or scarring in susceptible individuals.
Optimizing microneedling to maximize collagen growth
I will recommend practical steps before, during, and after treatment that enhance collagen output while minimizing complications. I emphasize that adherence to protocol and individualized planning matter most.
Pre-treatment optimization
I recommend stopping retinoids and certain exfoliants as advised by the provider, and managing active acne or infections prior to procedure. I also advise that smoking cessation and improving nutrition in the weeks leading up to treatment can improve healing.
In-procedure considerations
I stress the importance of appropriate anesthesia, depth selection, and technique to ensure consistent microchannel creation without overtraumatizing tissue. I also recommend using sterile technique and high-quality devices to minimize complications.
Post-treatment care to support collagen formation
Post-procedure, I advise gentle cleansing, sun protection, and appropriate topical support such as growth-factor serums or hyaluronic acid. I usually delay introduction of retinoids and aggressive actives until the epidermis has re-epithelialized to avoid irritation and interference with wound healing.
Topical agents and injectables that enhance collagen response
I will cover adjuncts with evidence for synergistic action and provide timing considerations to maximize benefit.
Platelet-rich plasma (PRP)
PRP contains concentrated growth factors that, when applied during or immediately after microneedling, can augment fibroblast activity. I note that randomized studies show improved clinical outcomes when PRP is combined with microneedling compared to microneedling alone.
Growth factor serums and peptides
Topical peptides and growth factor-containing serums can support matrix production during the proliferative phase. I caution that penetration depends on the timing relative to microchannel closure and the molecular size of the active ingredients.
Vitamin C and topical antioxidants
Ascorbic acid is a cofactor for collagen cross-linking and can support collagen maturation. I recommend introducing vitamin C serums after the epidermis has healed to minimize irritation and to maximize antioxidant protection.
Retinoids and timing
Retinoids are potent stimulators of dermal remodeling but can be irritating if applied too soon. I advise waiting until re-epithelialization is complete—often 7–14 days—before resuming retinoid therapy, with gradual reintroduction.
Safety, side effects, and how they affect collagen outcomes
I prioritize safety and will describe common side effects, risk mitigation, and how complications can delay or impair collagen formation.
Common side effects and expected healing
Temporary redness, swelling, and minor crusting are expected and do not indicate poor outcomes. I explain that these reactions are part of normal healing and should resolve without intervention in most cases.
Infection, hyperpigmentation, and scarring
In rare instances, infection, post-inflammatory hyperpigmentation (PIH), or hypertrophic scarring can occur and may impair collagen architecture. I emphasize early recognition and treatment—topical antibiotics, pigment control, or referral for scar management—to preserve long-term results.
Autoimmune concerns and contraindications
Patients with certain autoimmune disorders, active skin infections, or a tendency for keloids require careful evaluation. I routinely screen for contraindications and adjust or avoid microneedling when the risk outweighs the benefit.
Managing expectations and treatment planning
I will provide guidance on realistic goals and how to design a treatment plan that aligns with desired outcomes and timelines.
Setting realistic timelines
I clearly communicate that meaningful collagen-driven improvements usually appear within 1–3 months and peak at around 3–6 months. I always discuss that multiple sessions are often needed and that final remodeling continues over many months.
Individualized treatment plans
Treatment frequency, needle depth, and adjunctive therapies should be tailored to the individual’s anatomy, goals, and tolerance. I prefer to set incremental goals and reassess after each session to refine the plan.
Practical patient checklist: before and after treatment
I provide a brief checklist that I give patients to maximize safety and outcomes. This list is meant to be a practical, at-a-glance guide.
- Pre-treatment: Stop retinoids 3–7 days before (depending on strength), control active acne, avoid sunburn, maintain hydration, and discuss medications.
- Day of treatment: Arrange transportation if sedation is used, expect redness and swelling, and plan minimal social activities for 24–48 hours.
- Post-treatment: Use gentle cleanser, avoid makeup for 24 hours or as directed, apply sunscreen diligently, and delay potent actives until cleared by your provider.
- Long-term: Follow the recommended treatment series, avoid smoking, maintain sun protection, and schedule follow-ups.
Frequently asked questions (FAQ)
I will answer common patient queries succinctly to reduce uncertainty and facilitate informed consent.
When will I personally notice a difference?
Most patients I treat report subtle improvements within 4–8 weeks and more marked changes by 3 months. Final results often continue to improve up to six months after the last treatment.
Is more aggressive treatment always better for collagen growth?
No. I caution that more aggressive depth or excessive passes increase risk without guaranteeing proportionally better outcomes. The optimal treatment balances efficacy with safety and is individualized.
Can I combine microneedling with other cosmetic procedures?
Yes, combining with PRP, lasers, or fillers can be effective when sequenced properly. I recommend spacing procedures appropriately and discussing an integrated plan with your provider.
How many sessions will I need?
A typical starter series is three treatments spaced 4–6 weeks apart, but the total number depends on the indication and response. I personally reassess after each session and adapt the plan based on observed progress.
Case examples: practical timelines from my clinical practice
I will describe representative cases to illustrate realistic timelines and outcomes that reflect what I see in practice.
Case 1: Mild photoaging, 45-year-old woman
I treated a 45-year-old patient with three sessions at 4-week intervals using 1.0 mm depth for cheeks. She reported subtle texture improvement at 6 weeks and substantial tightening and reduced fine lines at 3 months, with continued improvement through month 6.
Case 2: Atrophic acne scarring, 30-year-old man
I used 1.5–2.0 mm depths for targeted scar remodeling over five sessions spaced 6 weeks apart. Early collagen deposition was apparent clinically at 8–12 weeks, with notable scar softening and volume restoration at 4–6 months.
Final recommendations for clinicians and patients
I will summarize practical, evidence-based recommendations so you can apply them confidently.
- Counsel patients that collagen growth is a biological process that takes time; expect progressive improvement rather than instant change.
- Tailor needle depth, session frequency, and adjunctive therapies to the clinical indication and patient factors.
- Use objective monitoring when possible, and combine with standardized photography for documentation.
- Prioritize safety: sterile technique, appropriate patient selection, and conservative escalation of treatment intensity.
Conclusion
I hope this detailed overview clarifies when microneedling results begin to show collagen growth and how the process evolves over time. I encourage patients and clinicians to set realistic timelines, to monitor progress methodically, and to use evidence-based adjuncts to maximize outcomes while maintaining safety.